This content is limited to our registered members
-
Access exclusive business services unlimited
-
Access valuable features : audio listening & tools sharing with your patients
-
Access more than 150 product sheets, dedicated to professionals
You already have an account ? login now
BIODERMA Congress Reports IMCAS 2023
Reports written by Dr. Laura Bouchard (Dermatologist, Finland) and Dr. Marta Cantarero (Dermatologist, Spain)
Related topics
Speakers: Dr. Ashraf Badawi and Dr. Muriel Creusot
Report written by Dr. Laura Bouchard
Dr. Ashraf Badawi presented the case of a young woman treated with a plasma pen on her neck who developed extensive scarring and hyperpigmentation post-treatment.
Plasma pens are increasingly popular, and more and more complications are erupting. Plasma pens are small cauterization instruments used on the surface of the skin, that cause a controlled burn and spread heat throughout the targeted area. They are promoted for eyelid lifts, wrinkle reduction and removal of moles, skin tags, scars and spots.
Complications include pain, swelling and redness of the treated area, burns, scarring, and hyperpigmentation. There is no control of the depth of treatment and they should only be used in very experienced hands if at all.
Health Canada has issued a Safety Alert and plasma pens are not authorized for sale in Canada.
The second case was a large Becker’s Nevus on the trunk of a young man who wanted reduction of the pigmentation.
The consensus of the panel was to persuade the patient not to have treatment because it is impossible to meet the expectations of the patient. However, all panel members recommended treatment of the hypertrichosis. Treatment parameters need not be conservative because hypopigmentation is not a problem in this case.
Dr. Muriel Creusot presented a case of severe hypopigmentation after facial hair removal with an alexandrite laser. The used settings were too high at 8 mm, 30 J/cm2. Mild hypopigmentation typically resolves by itself within 1 month to a year, but in this case the skin was sun damaged and the expectation is that the hypopigmentation will persist. Topical tacrolimus with sun exposure can be tried to stimulate melanogenesis. If the patient has a history of Koebner phenomenon with psoriasis, vitiligo or other skin condition, it is a contraindication for laser treatment.
Speaker: Dr. Anthony M. Rossi
Report written by Dr. Laura Bouchard
Fractional CO2 laser resurfacing pearls
In the session on CO2 lasers Dr Rossi presented a fresh of the oven study published in Lasers in Surgery and Medicine on procedures used by clinicians doing laser treatments (Practice patterns regarding combination treatments and laser and energy based devices: A Survey of American Society for Laser Medicine and Surgery Members. Dempsey et al. Lasers in Surgery and Medicine 2023).
Cleaning skin preparation
Ablative procedures
- Alcohol: 41%
- Chlorhexidine: 32%
- Hypochlorous acid: 11%
- Saline: 5%
- Cleanser + alcohol + chlorhexidine: 3%
- Soap & water + alcohol: 3%
- Biseptine: 3%
- Gentle cleanser + witch hazel: 3%
- No cleaning: 3%
Non-ablative procedures
- Alcohol: 51%
- Chlorhexidin: 22%
- Hypochlorous acid: 11%
- Saline: 5%
- Soap & water + alcohol: 3%
- Alcohol + hypochlorous acid: 3%
- Micellar water: 3%
- Gentle cleanser + witch hazel: 3%
- No cleaning: 3%
- HSV prophylaxis (ppx): 75% for ablative laser regardless of cold sore history
- 50% use one week antiviral course
- More than half do not limit antiviral ppx to perioral area
- Majority do not use antifungal ppx
- 2/3 use antibacterial ppx for ablative procedures of the face
- More than half apply petrolatum after ablative laser procedures
- Majority do not prime PIH prone skin prior to ablative laser procedures
- Most common priming regimen hydroquinone + retinol/retinoid + steroid
Speakers: Prof. Leonardo Marini, Dr. Diane Irvine (plastic surgeon) and Dr. François Will
Report written by Dr. Laura Bouchard
Photopeel for chrono-aging and photoaging
Prof Leonardo Marini from Trieste spoke about photopeel for chrono-aging and photoaging, which is his working horse.
Photopeel:
- IPL 500-950 nm
- Chemical peel with 15% TCA
- Mole protection prior to IPL
- Good results after just one treatment
He also uses a slightly more aggressive technique:
Fractional photo-peel:
- Warming the skin with short pulse 1064 nm laser, pulse duration 1.6 ms, 25-32 J/cm2
- 532 nm Q-switched laser spot-by-spot ablation of solar lentigines
- General pass with 530-750 nm IPL
- Fractional 2940 nm Er:YAG or fractional Q-switched YAG with low settings without bleeding
- 15% TCA ultra-fast chemical peel with Zimmer cooling
- Cold compresses and ice bags
Photodynamic photorejuvenation
PDT for Photodynamic photorejuvenation, uses more and more
- Same general sequence as fractional photo-peel but PDT instead of chemical peel
- 3 passes with 1064 nm 1.6 ms, 21.3 J/cm2
- 3 passes of fractional priming (pinpoint bleeding)
- Skin fluorescence is measured
- 0.5% 5-ALA liposome gel short incubation time (20-30 min), dark space
- 20 min blue LED light
- 30 min dark interval
- 20 min red LED light
- Cleansing with 1.5% H2O2
- 2 weeks after spring thermal water + hyaluronic acid
- 2 months after spring thermal water +0.05% retinoic acid + 50+SPF moisturizing cream
If you don’t have the devices
Instead of short pulse NdYAG for skin warming, an LED lamp 840 nm 20 min
Fractional laser: microdrilling
Q-switched laser: chemical peel 20% TCA
Fractional erbium laser as an alternative to upper blepharoplasty: indications and limitations
Dr Irvine showed clinical cases to show when to choose laser or surgery.
- Skin excess: surgery
- Skin creyping and wrinkles: laser
- Facial expression: surgery
- Periorbital volume deficit: surgery + fat grafting
- Residual skin: laser
- Mild brow lift: laser
- Low brows + excess skin: surgery +/- laser
- Little downtime: laser + fillers
- Bulging fat lower eyelids: surgery + repositioning of fat pad to tear through
Limitations of laser: less skin excess correction and not fat pad repositioning
Combination is best
Laser and toes beauty: treatment of ingrown nails
Local anesthesia: digital latero-distal block
- EMLA
- Distal hemi-block
- Lidocaïne 1% w/o epinephrine 2 ml (no tourniquet: larger vol)
Paronychium granuloma: CO2 laser vaporization
- Defocused
- 20-30 W
Lateral nail shelf: laser cutting lateral nail plate
- 20-30 W focused
- Removal of ingrown lateral tablet by a turning movement
Lateral matrix horn: CO2 laser vaporizatio
- CO2 laser defocused
- 25-30 W
- Lateral compression with the thumb to diminish bleeding
- Laser beam under the skin to the matrix horn (up to ~ 8 mm proximal to the nail fold)
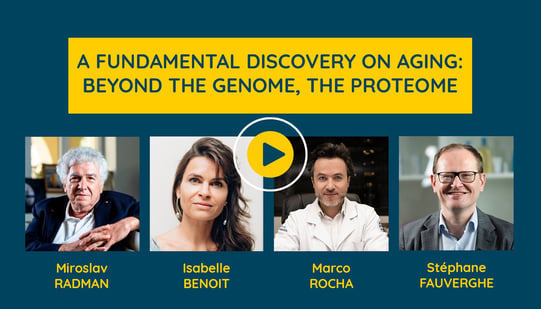
Speakers: Prof. Miroslav Radman (Croatia), Isabelle Benoit (NAOS Scientific Director, France) and Dr. Marco Rocha (Brazil)
Report written by Dr. Laura Bouchard
A proteome-centric view of aging and age-related diseases
A tin of meat was exposed to a dose of radiation that was thought to kill all known forms of life, but the meat subsequently spoiled, and the bacterium Deinococcus radiodurans was isolated.
Professor Radman has done groundbreaking research to understand what explains the extreme resilience of the bacterium and has found out with his colleagues that the capacity of D. radiodurans to endure oxidative stress is accounted for by a highly efficient protection against proteome, but not genome, damage and a DNA repair mechanism that permits it to reassemble its shattered genome in just a few hours (Zahradka et al., Nature 2006).
He evaluates that the impact of protein damage on the maintenance of life has been largely underestimated in biology and medicine and that the central dogma of molecular biology that DNA is at the base on everything should be revisited.
Proteins are in the middle of all life activities. We have about 21 000 protein species which carry on all life functions including repairing, replicating, copying, expressing genes. Genes are necessary as information to make proteins through RNA. Proteins are functions and the link between information and function is RNA. The activity of proteins is key to life.
Red blood cells have no DNA and yet function from 2 to 4 months. This is a redesign of the importance of these macromolecules in life. DNA isn’t anymore “the boss” of life and proteins “working class” molecules. Proteins maintain all life functions. Genes are important because there is information to make and refresh the proteins.
Furthermore, prof Radman studies now the mechanism of expression of aging and disease phenotypes. The long-term goal of this research is the mitigation of all age-related diseases by prevention and healing by phenotypic reversion. This approach aims to reduce disease initiation (at the genome level) and extend its latency period (at proteome level) to delay the onset of disease or revert the disease back to health.
Proteome alteration as the root-cause of skin aging
The NAOS has been closely collaborating with prof Miroslav Radman, a geneticist and molecular biologist recognized for some of his ground-breaking work on DNA repair, recombination and mutation and their impact on biological evolution and human health and establishing the role of oxidative damage to proteins in cellular resistance to radiation and desiccation, as well as in aging and age-related diseases
- Oxidative damage to the proteome is the root cause of ageing and thus also of skin ageing
- The skin is our biggest organ and is the most exposed to environmental stress
- Protection of the proteome of the skin: a breakthrough for age management strategy?
- Prof Radman’s research group has studied organisms able to sustain in an environment that should kill any form of life i.e. mostly bacteria that survived a lethal dose of radiation (Zahradka et al., Nature 2006)
- Deinococcus radiodurans were the first bacteria that were found to survive such conditions
- When its DNA is damaged, it is quickly fixed by inoxidable repairing proteins
- Proteins are the 2nd main component in the skin after water (15 - 27.5 % protein)
- Structural proteins of the skin: cells and tissues collagen, elastin, keratin
- Functional proteins of the skin: growth factors, enzymes, cytokines, hormones, aquaporins etc.
- Proteins provide all the functions of life in the skin >> Protein damage is the root cause of skin aging
- Proteome protection is the key to cellular longevity and healthy aging
- META THEORY: beyond most previous theories of aging
- Telomere attrition theory of aging: you can correlate the age of the length of its telomeres
- To protect the telomeres, you have to protect telomerase
- Telomerase is one of the least abundant proteins and among the most sensitive human proteins
- Link with inflammaging: chronic inflammation is initiated by inflammasomes and they in turn initiate a downstream inflammatory pathway: cytokines and interleukins
- Aberrant release of cytokines and interleukins induces a low-grade chronic inflammation called inflammaging that accelerates aging
- Sirtuin 2 inhibits low-grade inflammation and is also a protein
- Main damage to the proteome: carbonylation mediated by free radicals
- Carbonylation:
1. Inactivates proteins and makes them difficult to eliminate
2. Irreversible reaction
3. Formation of cellular aggregates that hinder cellular physiology
4. Acceleration of aging
- Carbonylation targets all layers of the skin
1. Stratum corneum: dehydration
2. Epidermis: loss of evenness, loss of radiance
3. Dermis: wrinkles, loss of firmness, loss of density
- Preventing protein carbonylation prevents skin aging: protection of the proteins and naturalization of free radicals
- In the nature chaperones protect the proteins
- Chaperones are overexpressed during stress, assist proper folding of the proteins and hide the sensitive amino acids to reduce the sensitivity to carbonylation
- Antioxidants can scavenge the free radicals and neutralize them
- NAOS Aging Science has found a naturally occurring chaperone and antioxidant in extremophilic bacteria Arthrobacter agilis isolated from a snowflake originally
- A. agilis:
1. Micro-organism capable of self-repair & survival in extreme conditions
2. Ultra-resistant to UV, Cold, oxidative stress
3. Synthesizes 6 antioxidant chaperones, Bacterioruberins
- Bacterioruberins at the same time chaperone-like & powerful antioxidants
- Bacterioruberins were extracted at NAOS Aging Science
- Chaperone-like activity of A. agilis Patent was tested in a specific “chaperone effect” – Heat Test against other antioxidants
1. Only A. agilis Patent had chaperone activity with 80% protection
- A. agilis had the strongest antioxidant power among tested known antioxidants
- Structural proteins protection (ex vivo): protects elastin from oxidative stress (UVA & pollution)
- Structural proteins protection (in vitro): A. agilis patent allows physical protection of DNA repair enzymes and protection of their functionality
- Protection against carbonylation (in vitro): protects proteins from carbonylation induced by UV, Blue light and pollution
- Ecobiologic breakthrough in skin care and aging science: both chaperone-like and antioxidant
Protection of the proteome: a new therapeutic way for healthy aging
- Our body has 16% protein
- 25 000 genes related to 1 million proteins
- ROS >> protein misfolding
- Chaperones are the proteins “quality control”
1. Folding of primary protein
2. Refolding a misfolding protein
- Damaged proteins can cause skin diseases: psoriasis, atopic dermatitis, skin cancer
- Denominators of aging
1. Genomic instability
2. Telomere attrition
3. Epigenetic alterations
4. Dysregulated nutrient sensing
5. Mitochondrial dysfunction
6. Cellular senescence & chronic inflammation
7. Stem cell exhaustion
8. Altered intercellular communication
9. Loss of protein homeostasis (proteostasis)
- External factors causing skin aging
1. Air pollution
2. Ozone
3. Thermal agents
4. UV radiation
- Internal factors causing skin aging
1. Produced during metabolism
2. Genetic factors
- Carbonylation and skin
1. Transepidermal water loss
2. Skin radiance
3. Collagen and elastin degradation
4. Inflammation
- Advanced glycation end products (AGEs)
1. Yellow discolorated skin
2. Loss of elasticity
3. Inflammatory pathways
- Targeting first step to slow down skin aging?
1. Target loss of proteases
- Growing evidence that protecting the proteome helps build and maintain tissues, may allow to slow down the process of aging
Speakers: Dr. Jill Waibel and Prof. Merete Haedersdal
Report written by Dr. Laura Bouchard
Combination CO2 and PLLA
- Uses both CO2 and Erbium lasers
- PLLA topical application
- Sometimes subcision and topical PLLA application
- Sometimes subcision, PLLA injection and topical application
Atrophic scars
- Rationale behind treatment: article on traumatic atrophic scars with one treatment (Rkein et al. Derm Surg 2014)
- 8 cc dilution: 6 cc sterile water + 2 cc lidocaine with epinephrine
Goal of Laser Treatment of Atrophic Scars
- Collagen stimulation within the atrophic areas: fractional CO2 and PLLA 1+1=4
- For relatively atrophic, shallow, or flat scars, non-ablative fractional appears to achieve similar results as ablative fractional
Energy Based Devices 2022 International Consensus Recommendations (Salameh et al., Lasers Surg Med 2022)
Treatment for deep atrophic scars
#1 Ablative fractional laser
#3 Subcision
Dr Waibel likes to combine treatments
Emerging Acne Scar Technique: multi procedural approach SAME DAY
- Atrophic boxscar: AFL & PLLA topically applied – 1-2 cc topically applied immediate post-operative
- Icepick scar: either punch biopsy or traditional CO2
- Rolling scar: AFL, subcision with PLLA injections
Settings, Tips, Pearls
AFL settings: measure depth with OCT – often between 500-1000 µm, density ~10% with ablative fractional
Prophylaxis case by case with antibiotics and antivirals
Close follow up
May need multiple treatments – usually start aggressive, then back down and do non-ablative fractional & inject PLLA
If active acne and acne scars ok to laser while on isotretinoin – in fact impression of improved result (Waldman et al. Dermatol Surg 2017; Spring et al. JAMA Dermatol 2017)
Laser assisted drug delivery (LADD) Signature Cocktails
The High Rise – Hypertrophic Scar: 5FU, TAC 10 mg/ml
Peaks and Valleys – Hypertrophic & Atrophic: PLLA, 5FU
The Wake Up Call – Hypertrophic & Hypopigmented: PLLA, TAC
The Depression – Atrophic & Hypopigmented: PLLA, Bimatoprost
Control visit in 3-6 months
Fractional CO2 or Microneedling-RF?
Study
- 15 patients
- Moderate to severe acne scars
- Split-face study
- Follow-up 2-4 d, 1 and 3 months
Multilayer technique
Results
- At 1 and 3 months: AFL and MNRF treatments are equally effective at improving texture
- AFL larger impact on disruption of skin integrity, both recovered at 1 month
- MNRF was more painful than AFL
Speakers: Dr. Kasper Kohler Alsing and Dr. Nicolas Kluger
Report written by Dr. Laura Bouchard
Cosmetic tattoos, ink chemistry and removal
Dr. Kohler from Copenhagen shared his experience with tattoo removal of cosmetic tattoos
- Found mostly in women
- No known prevalence
- Most common in Eastern Europe and South America
- New advanced for medical tattooing (nipple reconstruction after breast surgery, eyebrows in alopecia universalis, camouflage of scars)
- Majority of tattoo inks based on organic pigments (80%)
- Most problems with azo tattoos (red color, red allergies removal with surgical dermabrasion)
- Remaining 20% pigments iron oxide pigments
1. Ancient and cheap method to create colored pigments from natural sources
2. Promotes dull and natural color tones
3. Fits facial complexions – commonly used in cosmetic tattooing
4. High degree of iron
5. Contaminated from other metals
6. Can create artefacts in MRI
7. Reports of severe burning pain, transient erythema and oedema
8. Is not a contraindication for MRI but pain medication may be necessary
- Dr Kohler identified mineral oxides in permanent make-up inks by Mössbauer spectroscopy
1. Magnetite (black brown colour) most highly occurring magnetic mineral in the world
2. Hematite (brown rust colour) antiferromagnetic
3. Goethite (yellowish brown colour) weakly magnetic
- Crystals of iron oxides are taken in by macrophages
- Oxidation of iron over time
1. Colour shift from brown to red
- Dyschromia over time
1. Carbon black pigment in the outer skin diminished over time >> pigment in the lower dermis becomes bluish
- Titanium dioxide (white) used for lip highlighting
1. Hard to remove with laser
2. Can remain after red azo pigment has already faded
- Iron oxide pigment and Q-Switch Nd:YAG Laser
1. Can oxidize or create a reduction of these minerals
2. Paradoxical darkening of eyebrow tattoo
Take home message
- Iron oxides are common in PMU ink
- Iron oxides can interfere with MRI scanning
- Mineral oxides oxidize over time and change colour
- Q-Nd-YAG lasers can paradoxically darken pigment
Myths on tattoos and tattoo removal
Ten myths about tattooing
1. You can’t give blood when you are tattooed
4 months deferral after tattooing and piercing in most European countries
Study in the Netherlands:
- No increased risk of transfusion transmitted infections after tattooing, piercing or acupuncture when done in a parlour with professional rules of hygiene and asepsis
- No indication to propose a temporary deferral as 24% of them will not come back
- In the US no waiting period if tattoo done in a state-regulated facility
2. You cannot get an epidural analgesia if you have a lower back tattoo
Myth: no complication ever reported
3. “I breastfeed: I can get a tattoo”
It is suggested that mothers wait at least 9-12 months after birth, when the child is no longer dependent solely on breastmilk before getting a tattoo
4. “You cannot get a vaccination/jab in a tattoo”
- Choose the other arm
- Avoid the tattooed area if possible
- If tattoos cover both arms, choose a space within the tattoo without pigment if possible
However:
- No vaccination within a recent tattoo (<one month)
- No tattoo after vaccination (30-60 d window)
5. You cannot get a tattoo when…
- Venipuncture
- Peripheral venous catheter
- Central venous catheter
- Vascular access for hemodialysis
- Local or regional infiltration
- Spinal tap
6. A little ink test will tell me if I am allergic: NO
7. I can’t get a tattoo if I have nickel allergy: YES/NO
- Slightly higher prevalence of positive patch test for nickel sulfate in tattoo reactions
- Piercing can be a cofounding factor
- Role in case of acute eczema after tattooing?
- The author does not contraindicate tattooing to a sensitized individual
- Recommend a black tattoo if patient wants to avoid the risk
8. Tattoo will give cancer: NO
- Review in 2012: no difference (Kluger & Koljonen, Lancet Oncology 2012)
- Mouse study with black ink: the area around the tattoo was more prone to skin cancer than the tattooed area (Lerche et al., Photodermatol Photoimmunol Photomed 2015)
- Mouse study with red ink: red tattoos exposed to UVR showed faster tumor onset regarding the third tumor (Lerche et al. Experimental Dermatology 2017)
- 34 melanoma cases reported between 1939 and 2019
9. Cream can removed my tattoos: NO
10. My new method is better than laser and surgery: NO
Speakers: Prof. Nicolas Dupin (University Central Hospital Paris Centre - Hôpital Cochin) and Prof. Marie Beylot Barry (University hospital of Bordeaux)
Report written by Dr. Laura Bouchard
Blocking inflammation induced by C. acnes
Prof Dupin’s research group have worked for already 20 years on how c. acnes is implicated in inflammation in acne.
Meclozine a new anti-inflammatory molecule to treat acne
- Found by screening well known molecules
- Antihistaminic drug
- Reduced inflammation induced by c. acnes
- No toxicity on keratinocytes
- Reduction of cytokines
- Reduction of transcripts of IL8 and IL1ß
- A “home-made” meclozine 1% or 2% gel reduced inflammation in mice injected with c. acnes
- Pilot study:
1. 60 patients
30 meclozine gel 2%
30 vehicle alone
2. At 12 weeks nearly 60% in the treatment group evaluated a decrease of acne symptoms vs 28% in the vehicle group
3. Acne severity index (ASI)
20% reduction vs 8% (p=0.0004)
73% improvement vs 43% (p=0.03)
4. No significant side-effects
How to manage complex acne
Chronic recurrent acne
Acne in adult women (>25 y)
- Multiple flare-ups
- Multiple previous courses of antibiotics
- +/- intolerance to cyclins
- 20-30% of adult women
- Particular “U” shaped location
- Mostly inflammatory, mostly mild to moderate, strong impact on quality of life
- Skin intolerance
- Insidious scarring evolution
Factors affecting choice of treatment
- Severity of acne
- Hyperandrogenism?
- Triggering/worsening factors? (including IUDs)
- Response and tolerance / previous treatments
- Frequency of resurrences
- Psychological and social impact
- Risk of scarring
- Pregnancy desire
Low-dose isotretinoin
Study from Rademaker et al., JEADV 2014
- Moderate acne
- Improvement after 4 weeks
- 62% no lesions at 32 weeks
- Improvement of quality of life
- Good tolerance
- 30-36 months follow-up in 38 patients
60% relapsed
After ~7 months of discontinuation
Mild relapse but 48% resumed low-dose isotretinoin daily or twice a week
- Low-dose: 5-10 mg/d
- Duration? Necessary to reach total cumulative dose 120 mg/kg..?
- Continuous treatment (daily, not twice weekly) vs intermittent (“stop and go”) sessions?
- Frequent recurrences
- Monthly pregnancy control and contraception needed
- Pregnancy desire problem
Oral contraceptives
- Delayed but prolonged positive effect on acne
- Not recommended outside need for contraception in the French Guidelines
- Low thromboembolic risk but should be considered in this adult population
- Oral combined estro-progestins often not wanted by adult patients
- IUDs or implants preferred in this population but may worsen acne
Spironolactone
- Not approved but option for acne in North American Guidelines
- Tolerance?
- Irregular cycles, breast tension, low libido, frequent hypotension, headaches
- Contraindicated during pregnancy
- Hyperkalemia but no monitoring required < 45y
- Efficacy:
- Cochrane review conclusion mostly negative
- Recent review probable efficacy at 200 mg/d
- Retrospective study in large population (n=403) Garg et al. J Am Acad Dermatol 2021
- 2008-2019: 403 women, median age 24y
- 100 and then 150-200 mg/d ++
- Half the patients continue the treatment after 24 months and half have no more lesions
- Awaiting results of two controlled studies UK and France
Highly inflammatory acne
- Very inflammatory acne
- Acne fulminans (AF) spontaneous or after introduction of isotretinoin (iso) (with or without systemic symptoms)
How to treat
Evidence-based recommendation for management of acne fulminans Greywal et al. J Am Acad Dermatol 2017
- Oral corticosteroids 0.5-1 mg/kg/d 2-4 weeks depending on systemic signs until lesions heal
- Then low dose isotretinoin 0.1 mg/kg/d
- If AF on iso, stop and resume after disappearance of crusts and hemorrhagic lesions
- Progressive increase iso dose according to tolerance + progressive tapering of corticosteroids (4 to 8 weeks)
- Super-potent corticosteroid cream on granulation tissue
In addition
Intralesional delayed corticosteroid injections into large cysts and nodules especially in acne conglobate
- Anti-inflammatory action, reduction of scarring evolution
- Limited literature
- Shared experience triamcinolone 2.5-10 mg/ml, 0.1-0.25 ml/lesion
If previous treatment protocol does not help
- Anti-TNF
- Apremilast
- (Colchicine)
Personal patient case of iso induced AF worsening despite low-dose iso and corticosteroids
- Oral CS 1 mg/kg/d + stop iso
- Azithromycine 500 mg/dn1-3 days per week for 6 months
- Oral corticosteroid reduced and stopped in 3 months
- No recurrence of AF in 3y follow-up
Speakers: Dr. César González, Dr. Lim Tingsong, Dr. Rym Benmously Mlika, Dr. Fotini Bageorgou, Dr. Teresita Santillán Ferrariz, Dr. Ayata Nishikawa, Dr. Arisa Ortiz and Dr. Leonardo Marini
Report written by Dr. Marta Cantarero
Updates on melasma
Dr César González from Colombia, known as “Dr Spots”, was the first speaker on the important and frequently discussed topic of approaches to melasma.
The Royal Spanish Academy, the leading official authority on the Spanish language, erroneously defines melasma as “irregular dark spots that occur most commonly on the face during pregnancy and illness.” This definition is incorrect. It’s important to understand that melasma is a complex and multifactorial condition that is not due to a single cause, and that a number of different cells are involved in it.
Dr César González raises the question of why current protocols for the use of oral tranexamic acid are only for a period of 3 months if we are treating a chronic disease. He suggests that we should review and study the data to offer this treatment for a longer duration while ensuring complete safety. In his opinion, use of lasers should be minimal, and they should not be used if there is any doubt.
A key point about melasma is that it is a cutaneous pathology in which photoageing is present and should therefore also be part of the treatment, alongside all the treatments we consider in the clinical context.
Targeted melasma management
Dr Lim Tingsong from Malaysia gave a talk explaining the pathogenesis of melasma.
Melasma is an acquired form of hyperpigmentation in which there are changes in fibroblasts and endothelial cells, with factors like genetics, ultraviolet radiation, heat and hormones potentially contributing to its development. Ultraviolet radiation promotes activation of tyrosinase expression, an early step in melanin formation. In addition, it has been confirmed that skin with melasma shows greater VEGF activation, which implicates vascularisation in its pathogenesis. Furthermore, damage in the basement membrane facilitates the migration of melanocytes to the dermis, thereby producing constant hyperpigmentation.
We should also consider the role of senescent fibroblasts as a contributing factor in melasma.
Severe melasma should be treated with combined treatments since it is a multifactorial process.
We must bear in mind that the role of lasers needs to be studied very thoroughly, due to the hypopigmentation or rebound effect it can have in melasma.
Melasma: a better understanding of the use of tranexamic acid
Dr Rym Benmously Mlika from Tunisia is the president of the Laser group in her country. She presented different clinical cases with real patients in which she showed how melasma appears in dermatoscopy as a light brown colour together with a globular reticulum pattern in the epidermal zone.
Melasma results from the interaction of ultraviolet radiation, drugs, hormones and genetic factors that influence keratinocytes, melanocytes, fibroblasts and endothelial cells. In addition, there are 300 genes that affect not only melanocytes, but also components of the dermis.
Histologically, the signs we see with melasma are solar elastosis, disruption of the basement layer, increased vascularisation and an increase in mast cells.
We also know that fibroblasts secrete factors involved in the pathogenesis of melasma.
Tranexamic acid is a fibrinolytic agent with a long history of use for bleeding, as well as an inhibitor of plasmin which prevents fibrinolysis, thereby reducing bleeding.
Dr Rym presented a number of clinical studies on oral, intralesional and topical use of tranexamic acid, with topical use being the least effective. More exhaustive protocols are still needed for its use in aesthetic treatments. Interlesional application of tranexamic acid can be considered as safe, effective and well-tolerated.
Differential diagnosis of melasma
Dr Fotini Bageorgou from Greece described melasma as a persistent pathology that requires maintenance and long-term treatment in conjunction with innovative treatments. The ideal treatment plan is maintenance. But not everything is melasma, and we need to differentiate it from other pathologies with which it can often be confused. Dr Fotini provided us with a differential diagnosis for pathologies which may appear to be melasma but are not. Among them, the most frequent is post-inflammatory hyperpigmentation, for which she uses superficial peelings together with topical corticosteroids and sun protection. Riehl melanosis occurs in middle-aged women, and involves the appearance of brown spots in a reticulated pattern in the neck area, where its cause is multifactorial. Erythromelanosis follicularis faciei is rare, and causes dyschromia with erythema and papules on the face and neck in men. It is associated with keratosis pilaris. The hyperpigmentation produced by amiodarone is characteristic, with a bluish tone in the face. Porphyria cutanea tarda presents with facial hyperkeratosis as well as blisters, primarily on the backs of the hands. In Addison’s disease, we know that there is a generalised hyperpigmentation primarily affecting photoexposed areas, and we also need to examine the mucosa. The ochronosis produced mainly by the use of topical hydroquinone is irreversible, especially in dark phototypes. Linea fusca is a brown line in the anterior hairline area. Hori’s nevus is a facial nevus that is the most common form of acquired facial dermal melanocytosis, and primarily affects Asian women.
Another curiosity is reversible facial hyperpigmentation associated with vitamin B12 deficiency. It is a generalised hyperpigmentation, but is more prominent in the middle third of the face.
PRP for melasma
Dr Teresita Santillán Ferrariz considers PRP as a third line of treatment for melasma, and thus as a helper for all forms of treatment. PRP (or platelet-rich concentrate) is an autologous product containing growth factors that can stimulate and accelerate tissue repair. Dr Santillán showed us how PRP is injected into a patient’s face with intradermal injections for 6 weeks at intervals of every 2-4 weeks, then repeating this series of injections at 6 months and one year. PRP acts on epithelisation, extracellular matrix production, angiogenesis and tissue maturation. The other important point is that PRP is a tyrosinase inhibitor via TGF-b1. PRP is therefore a good alternative option for long-term treatment of melasma.
Radiofrequency microneedling in patients with melasma
Dr Ayata Nishikawa, a dermatologist from Japan, spoke about the effectiveness of pulsed fractional RF in melasma treatment since 2020. This technique can be effective against refractory melasma and also improves skin quality: pores, wrinkles and rosacea. Her research group studied 29 patients treated with this technique without any other combinations, measuring variables such as Visia. No side effects were observed. The results showed reduced pigmentation of the melasma and increased patient satisfaction.
Updates on combined treatments for melasma
Dr Arisa Ortiz from San Diego explained that combined treatment, rather than monotherapy, is essential. The combination of treatments can include lightening agents, chemical peelings, microdermabrasion, lasers and oral medication. Lightening agents other than hydroquinone include peroxidase, oligopeptides, Lytera, Melaplex and resorcinol. Cysteamine, tranexamic acid and oral antioxidants such as glutathione. Among lasers, Dr Ortiz recommends the Diodo 1927 nm fractional laser for its low rebound risk. We also know that melasma has a vascular component, so lasers can also help us in this regard. Dr Ortiz applies clobetasol just after the laser because it helps to reduce inflammation and posterior hyperpigmentation. With regard to oral treatments, she talked about polypodium leucotomus and explained its ability to block ultraviolet radiation and repair damage to cellular DNA. As for tranexamic acid, we know that it is an antifibrinolytic and procoagulant and that it inhibits melanogenesis and neovascularisation. Keep in mind which patients are at risk from treatment with tranexamic acid: smokers, contraceptives, neoplasias, heart failure. Consensus on the keys to treatment.
Melasma: what to do and what not to do
Dr Leonardo Marini explained what not to do in melasma treatment by presenting reported cases in which melasma symptoms got worse. He started his talk by noting that we have to be able to explain to patients that there is no effective cure and that the treatment will be lifelong. Therefore, the patient has to be aware of this and of the constant need for treatment. The treatments that are recommended are gentle, early treatments, and always in combination. Conversely, treatments that are non recommended are aggressive ones like ablative lasers or chronic hydroquinone application.
Speakers: Dr. Delphine Kerob, Dr. Behrooz Kasraee and Dr. Sabine Zenker
Report written by Dr. Marta Cantarero
Melanogenesis and pigmentary disorders
Dr Delphine Kerob, a dermatologist at the Saint-Louis hospital in Paris, explained how pigmentary disorders are among the most frequently occurring dermatological pathologies. They are more common in people with darker phototypes. They are also a source of stigmatisation and lead to strong demand for treatment.
Pigmentary disorders can be classified into hyperpigmentation and hypopigmentation. The colour of our skin results from the contribution of different pigments such as melanin, haemoglobin, carotenoids, and bilirubin. There are three important enzymes in the process of melanin synthesis: tyrosinase, tyrosinase-related protein 1, and the DCT/TYRP2 complex.
The melanogenesis process can be affected by genetic problems such as Carney syndrome, in which we see hyperactivation; in Peutz-Jeghers syndrome and LEOPARD syndrome, which are RASopathies; and in oculocutaneous albinism, Waardenburg syndrome, and piebaldism.
Non-genetic factors can be found in the clinical context, with inflammation, oxidative stress, fibroblasts, sebocytes and keratinocytes all having a potential influence, and all requiring treatment as a whole.
When can a depigmenting agent be considered effective?
Dr Behrooz Kasraee explained the various depigmenting agents, which are classified into phenolic, carboxylic, thiol and other agents. She explained some of them to us, such as hydroquinone, tranexamic acid, and innovative amino acid treatments.
- Hydroquinone is the gold standard for treating melasma. It is more effective in combination with formulas. It affects melanocytes and is toxic to them, and can cause facial irritation, as well as ochronosis in the long term, and should therefore not be continued for long-term treatment. It is suspected to have carcinogenic properties in vivo.
- Tranexamic acid is an analogue of lysine. It can be applied topically with low efficacy, or taken intradermally or orally. It inhibits inflammation, which is involved in melanogenesis.
- Cysteamine is produced physiologically and is a powerful antioxidant that inhibits melanogenesis, is safe for long-term use, and effective with pigmentary disorders. It may cause irritation.
- A new option is isobionicamide, which is a melanosome transport inhibitor and inhibits tyrosinase.
Choosing cosmoceuticals for use with melasma
Dr Sabine Zenker, a dermatologist from Germany, told us about new developments in the pathogenesis of melasma and topical application strategies.
- Retinol is a precursor of retinoic acid which can thicken the epidermis and promote proliferation of the dermis, and has both anti-inflammatory and anti-pigmentation effects.
- Tranexamic acid can reduce angiogenesis and inflammation, and also reduces histamine.
- Antioxidants like ibedenone and glutathione are used as pigmentation inhibitors, as is melatonin, a powerful antioxidant which also has a depigmenting effect.
- Other acids used include alpha hydroxy acids, kojic acid and ferulic acid, all of which are antioxidants and have anti-inflammatory effects.
- Niacinamide inhibits melanosome transport.
A combination of all of these is a good treatment alternative, as is melaphenone, reducing tyrosinase by 55%.
Speakers: Dr. Alexandra Mora Hernández, Dr. Frédéric Braccini, Dr. Sergio Omar Escobar and Dr. Frank Rosengaus
Report written by Dr. Marta Cantarero
Surgical rhinoplasty
Dr Alexandra Mora Hernández, plastic surgeon, spoke about the possible risks of rhinoplasty including asymmetries, persistent occasional pain, visible or hypertrophic scars, perforation of the septum or the need for additional surgery. She explained the different surgical techniques used in rhinoplasty, illustrating them with difficult cases and possible solutions. In conclusion, the take-home message is that sometimes it’s better to start with a rhinoplasty than a series of multiple rhinomodelings.
Medical rhinoplasty
Dr Frédéric Braccini from France discussed his 15 years of experience in medical rhinoplasty, i.e. rhinomodeling. He began his talk by explaining that hyaluronic acid fillers are like an airbag against surgical rhinoplasty, and in many cases are used before surgery. At present, hyaluronic acid is the only product that should be used for nose reshaping. In addition, the hyaluronic acid we use should be highly reticulated. To ensure a safe technique, we must be familiar with the product, the anatomy, the indications, and how to manage the technique. We know that the nose is an area that is frequently susceptible to necrosis. Dr Braccini explained his infiltration techniques with examples from various patients. He uses 25G cannulas for the nasal dorsum. He also explained techniques for opening the nasal ala.
Risks and treatment of nasal arterial occlusion
Dr Sergio Omar Escobar from Argentina began by explaining the anatomy of nasal vascularisation, emphasising the importance of the dorsal nasal artery, the angular artery, the infraorbital artery and its anastomoses, the lateral nasal artery, the labial artery, the facial artery and the columellar artery. He presented videos explaining how the hyaluronic acid filler remains in place once injected.
He also explained a vitally important protocol in case of vascular occlusion:
400 to 1500 IU in the area, with massage repeated every 4 hours for the next 4 days.
Rhinosculpting: using surgical concepts for non-surgical techniques
Dr Frank Rosengaus presented a scientific article and explained the differences between cannulas and needles. He favours needles, and even stated that there are more cases of side effects with cannulas than with needles. The nose gives us an understanding of the mid and lower area of the face. Therefore, the initial evaluation is most important. We need to take the nasal angles into account. He again emphasised the importance of the vascularisation of the nose and its anastomoses, especially with the ophthalmic artery.
The choice of product should be cohesive, with minimal integration and a high G prime rating. For a nose that has already undergone a previous rhinoplasty, it is better to use a hyaluronic acid with a lower G prime.
Speakers: Dr. Tahera Bhojani Lynch, Dr. Tom S. Decates, Dr. Editta Buttura da Patro, Dr. Patrick J. Treacy and Dr. Hema Sundaram
Report written by Dr. Marta Cantarero
Which is safer: cannulas or needles?
Dr Tahera Bhojani Lynch spoke about real experiences with the use of cannulas or needles. The most important point to be clear about is the ability to recognise vascular occlusion and the first signs of pallor in case of arterial embolism, and of venous regurgitation in case of venous stasis. It is clear that the risk of occlusion can be greater depending on the entry zone, quantity, and injection force – it is important to inject slowly. If the embolism is anterograde, it will cause skin necrosis, but if it is retrograde, it can cause blindness. The doctor explained that skin necrosis usually resolves spontaneously within 6 weeks due to anastomoses.
The origin of complications with fillers
Dr Tom S. Decates from the Netherlands presented clinical cases of complications with non-absorbable fillers. We must bear in mind that complications are also due to genetic predisposition, immunity and bacteria. The cause of these abscesses is probably the biofilm that surrounds them and makes them resistant to antibiotic treatments; as a result, we sometimes need to open them surgically to clean them out.
Preventing complications with hyaluronic acid treatments
Dr Editta Buttura da Patro is a maxillofacial surgeon, and spoke mainly about dental issues in patients. We need to evaluate the patient carefully, because sometimes the treatment they need is not a hyaluronic acid filler but a maxillofacial surgery due to poor dental occlusion leading to movement and soft tissue loss. The doctor therefore explained that a good evaluation is essential, and that practitioners should ask a maxillofacial specialist for help in case of doubt, given that a change in muscle dynamics due to hyaluronic acid can change the aesthetics of our smile. Her take-home message was that not all of our patients require an aesthetic or surgical procedure, and that we need to evaluate whether it will really improve their appearance. Our obligation is to understand what the problem is, what the anatomical causes in order to potentially resolve them, and to be responsible for educating the patient about an objective outcome.
Treating nodules after covid vaccination
Dr Patrick J Treacy explained how treatment should proceed for the inflammatory lesions that we have been seeing after covid vaccinations. The initial treatment should be with antibiotics such as macrolidea (clarithromycin 500mg twice daily or doxycycline 100mg 2x/day). After two weeks, we can add dexamethasone 4mg/day for one week. If no improvement is seen after four weeks, we can consider treatment with hyaluronidase.
It’s important to remember that we’re talking about type IV reactions causing granulomas. For treatment, patients have been given antihistamines, 5-fluorouracil, hyaluronidase and intralesional corticosteroids. It usually occurs in patients who have had hyaluronic acid injections of various types. Dr Treacy uses methrotrexate for his treatments. It’s a drug that we should be familiar with for its side effects, primarily hepatotoxicity and pulmonary fibrosis.
Topical hyaluronidase
Dr Hema Sundaram presented an innovative pilot study investigating topical hyaluronidase. Hyaluronidase is an enzyme that depolymerises hyaluronic acid in human cells. Topical treatments with hyaluronidase allow us to provide a non-invasive treatment with excellent tolerance and no side effects in a cosmetic product. The main indications are the periorbicular and perioral areas, although it has also been used for malar festoons. The Vectra assessment technique shows a reduction of 0.27cc in hyaluronic acid after application of hyaluronidase, in a study of 18 patients with irregularities after hyaluronic acid injections. The results showed 15 of these patients with improved uniformity. Dr Sundaram showed us clinical photos documenting this improvement. This product may be widely used in the future, so we should all be familiar with it.
Speakers: Dr. Roberto Dell’Avanzato, Dr. Aslican Cakkalkurt, Dr. Finesse Angelica, Dr. Nenad Stankovic, Dr. Anna Grodecka, Dr. Ariel Romeo, Dr. Tzachi Shelkovitz and Dr. André Ferrao
Report written by Dr. Marta Cantarero
Treating complications with intralesional laser
Dr Roberto Dell’Avanzato from Italy described how hyaluronic acid fillers can cause nodules and superinfected granulomas. To deal with this problem, he showed us how his team uses lasers with the Marangoni technique. Before using laser, all patients must be treated with azithromycin 500mg per day for 3 days every 4-6 weeks, levofloxacin 500mg 1x/day, proton pump inhibitors and probiotics. The effect of the intralesional laser is essentially to eliminate biofilm. We need to disintegrate the polymers, eradicate the infection and eliminate the inflammatory cells, and all of this is achieved with intralesional laser. Dr Dell’Avanzato showed us videos of his technique. It does not require anaesthetic, and provides immediate relief by reducing nodules and controlling inflammation.
Managing complications with hyperbaric oxygen therapy
Dr Aslican Cakkalkurt showed us how hyperbaric oxygen chambers are used as a complementary treatment for complications after hyaluronic acid filler injections. Some of the indications for use of the hyperbaric chamber are necrotising soft tissue infections, acute traumatic ischaemia, nonhealing wounds, arterial insufficiency, flaps with vascular involvement, and retinal vascular occlusion. Hyperbaric oxygen produces improved perfusion, reduced secretion of inflammatory cytokines, increased collagen production, increased angiogenesis and increased leukocyte and macrophage function. Dr Cakkalkurt presented 4 clinical cases showing clear improvement of complications with the hyperbaric chamber, but always as a complementary treatment, which we need to keep in mind.
Treating refractory blepharoptosis with oral pyridostigmine
Dr Finesse Angelica from the Philippines discussed one of the most common side effects after botulinum toxin injections, namely palpebral ptosis. Blepharoptosis results from dysfunction of one or both of the levator muscles of the upper eyelids. She showed us the three grades of blepharoptosis: grade 1 (minimal), less than 3mm; grade 2 (moderate), 3-4mm; and grade 3 (severe), greater than 4 mm. It’s also important to know that blepharoptosis can cause blurred vision and increased tear production. Acquired blepharoptosis is produced by a diffusion of the toxin through the orbital septum to the levator muscle of the eyelid, causing the muscle to become fatigued. Onset is usually 3 to 14 days after injection, and usually resolves on its own in 3-4 months. The conventional treatment is brimonidine eye drops, but pyridostigmine can be used in refractory cases. Pyridostigmine is a cholinergic inhibitor that prolongs the presence of acetylcholine in the neuromuscular junction, is category C for pregnancy risk, and its effects are reversible. It should not be used in case of intestinal or bladder obstruction, and should be used with caution in pregnant patients or those with asthma. Its effect is amplified by morphine and barbiturate derivatives. In the eye, it causes miosis and reduces intraocular pressure. In adults, the recommended dose is 60mg oral x 6 weeks.
Saint Hyaluronidase
Dr Nenad Stankovic spoke about the much-feared vascular occlusions that can occur with hyaluronic acid injections. Hyaluronidase can come to our rescue in a huge number of situations, so everyone should be familiar with it. Side effects, though rare, include stinging at the injection site, pain, erythema, allergic and anaphylactic reactions. A control test must be performed before using it. Inject 0.05 cc to form a papule on the forearm and wait 15 minutes; if it is then larger than 5mm in diameter, then the test result is positive.
If arterial occlusion is suspected, take photos and videos of the area, disinfect it, and inject 1500 units of hyaluronidase diluted in 1 ml of NaCL (or in lidocaine). Infiltrate the entire affected area and prepare another vial in case it becomes necessary. Administer another equal dose after 15 minutes, then massage vigorously. Compare with the earlier photo and video. Keep the stages of ischaemia in mind: pallor, reticular livedo, pustules, coagulation and crust. Pallor and livedo do not require treatment, but treatment is required from the pustule stage onward. If we are only diluting nodules, inject 0.02cc per point.
Vascular complications after polycaprolactone filler injections
Dr Anna Grodecka, a dermatologist in Poland, presented the case of a patient who is also a doctor and a friend of hers, and described the patient’s risk factors after a suspected vascular occlusion. Treatment started with hot massage, aspirin 500mg and prednisone 40mg oral, followed immediately by injection of a vial of hyaluronidase. The patient then went into the hyperbaric chamber, then repeated with two more vials of hyaluronidase, then PRP and betamethasone infiltration. Finally the complication resolved with subsequent approval. These cases teach us how our colleagues have handled these situations and how we can deal with them ourselves.
Treatment of filler inflammation after covid or vaccination
Dr Ariel Romeo from Spain showed us photos of tissue inflammation in dermal filler areas months after a covid infection or after vaccination. Clinically, complications such as erythema, painful nodules, induration, palpebral oedema, and stinging sensations are observed. Initial treatment should be deflazacort, macrolides or quinolones, cetirizine, hyaluronidase and intralesional triamcinolone. However, the most important factor is prevention. We should only inject if there are no signs of local infection, and wait 2-3 weeks pre- or post-vaccination.
For small nodules, it is recommended to wait, but treatment is recommended for larger nodules, especially in case of pain, oedema and erythema.
Dr Romeo provided exact doses: deflazacort 1 mg/kg/day, macrolides and quinolones, cetirizine 20mg/day, lisinopril 5mg/12h, hyaluronidase and intralesional triamcinolone.
Managing facial fillers
Dr Tzachi Shelkovitz from Israel explained his personal treatment protocols for managing long-term inflammation and nodules after filler injections. He explained that the protocols he follows are his own, and that he does not follow any clinical guidelines. He presented various clinical cases of nodules and inflamed granulomas after injection of hyaluronic acid fillers, for which the doctor injected 2cc of 5FU together with 2cc of lidocaine, after which patients reported an improvement. In addition, he always follows with augmentin 875mg 1x/day continuously and prednisone 20mg/day.
Treatment of complications with permanent fillers
Dr André Ferrao from Brazil presented various cases of permanent fillers performed a few years ago with silicone. Siliconoma formation causes granulomatous nodules in conjunction with an inflammatory reaction and diffuse erythema combined with dyschromia. Patients also receive treatment with oral corticosteroids and magistral formulas for dyschromia. Other cases presented by the doctor require surgical resection of the granulomas, combined with lifting techniques.
Speakers: Dr. Steven Dayan, Dr. Eqram Rahman, Dr. Michael Gold, Dr. Meelad Habib and Dr. Oliver Philip Kreyden
Report written by Dr. Marta Cantarero
Efficacy of Botox dose vs. placebo in masseter muscle treatments
Dr Steven Dayan from San Diego explained the use of botulinum toxin in treatments targeting the masseter muscle. We can use botulinum toxin treatments to successfully treat this powerful muscle that is responsible for mastication. Masseter muscle treatments can achieve an inversion of the facial triangle for a younger-looking face. Dr Dayan compared patients treated with 48 units of botulinum toxin vs. 72 units of botulinum toxin and studied the duration and effects in both cases. The end result was a significant reduction and improvement in muscle contraction at 180 days after the treatments seen by investigators and participants. All patients were more satisfied after the treatment. Both doses (48 and 72 units) are well-tolerated in adults.
Miracles with botulinum toxin A
Dr Eqram Rahman presented a prospective pilot study that examined 10 patients with intradermal botulinum toxin injections over the whole facial surface. They were injected with 20 units in 1 ml of saline solution with the goal of reducing facial seborrhoea and improving pore visibility and rosacea in the T zone in comparison with the rest of the facial surface, including the nose. The results showed a reduction in sebum production, a decrease in pore size, reduced erythema and somewhat fewer wrinkles. Dr Rahman also introduced the concept of micro-RNA, which showed a gradual increase in all patients.
Comparing botulinum toxins
Dr Michael Gold discussed the various botulinum toxins available on the market. He spoke about the following types: onabotulinum toxin A, abobotulinum toxin A, incobotulinum toxin A, prabotulinum toxin A, daxibotulinum toxin A, letibotulinum toxin A, and relabotulinum toxin A. He showed us studies starting from 2019 that compared all of these toxins. The conclusions were very similar for all of them. There are no toxins that are better than others. Some appear to last longer, some are quicker to achieve results, but none of the differences are statistically significant. A new toxin, daxibotulinum toxin A, has arrived on the market under the brand name Daxxify, and shows similar results to the others. Dr Gold also talked about the liquid toxin marketed by Galderma which does not require reconstitution and is therefore more convenient, but it causes stinging which leads to tolerance problems in patients.
Clinical uses of botulinum toxin
Dr Meelad Habib talked about non-cosmetic clinical uses of botulinum toxin. It was a very interesting talk that showed a wide variety of uses for botulinum toxin in different medical specialisations. We learned about its use in Raynaud’s syndrome, which manifests with triphasic colouration (white, red and blue) due to transitory vasospasms. He presented a double-blind pilot study which showed improvement after injection of botulinum toxin and no vasospasms, and superficial vascularisation of the skin also increased significantly. Another interesting use is in digital ulcers to improve pain symptoms and vascularisation of the affected area. However, no significant improvement was seen in patients with scleroderma with associated Reynaud’s syndrome.
Botulinum toxin for use in hyperhidrosis
Dr Oliver Philip Kreyden, one of the world’s pioneers in the use of botulinum toxin for hyperhidrosis, talked about the use of this toxin for hyperhidrosis not only in the axillary or palmoplantar regions, but also in other areas like the nose, chin, forehead, backs of the feet, and the anal, parotid, malar, intermammary, submammary, and perianal regions. One of the disadvantages of botulinum toxin injections in the palms and soles of the feet is pain. Nerve-block anaesthesia leads to multiple side effects and is not commonly used. One therapeutic tip from the doctor’s videos is the use of cryotherapy just before the injection to mitigate the associated pain.
Speakers: Dr. Marcin Ambroziak, Dr. Sahar Ghannam and Dr. André Braz
Report written by Dr. Marta Cantarero
Russian lips
Dr Marcin Ambroziak from Poland showed us the different techniques for doing Russian lips, wide and voluminous lips that certain actresses have made fashionable. We have the micropuncture technique: a large number of punctures from the upper and lower vermilion to the submucosa, and finishing with the commissures and the two upper points. Or the microtriangle technique, applied in the same way as the previous technique, but forming miniature triangles on the lip and finishing in the same way. The outer edge is the only safe area of the lip. Keep in mind that deep injections in the lips are the most dangerous.
Middle Eastern lips
Dr Sahar Ghannam is the author of the article “Lip harmony and rejuvenation” published last year, a study with 70 patients in which lip rejuvenation techniques were used. Before puncturing, it is very important to know the precise vascularisation of the labial artery and of the targeted area, due to the risk of vascular occlusion. Dr Ghannam also presented articles showing what to do in such cases. The injected product and the arteries are extremely close. The doctor emphasised that less is more, and that safety should always be our top priority.
Brazilian lips
Dr André Braz from Brazil is the author of multiple books on facial anatomy, and illustrated his talk with real clinical cases and their correspondences in cadavers. It is important to remember that the labial artery is found in the submucosa in 58% of patients, in the intramuscular layer in 36%, and in the subcutaneous layer in 5%. Dr Braz showed us different videos using cannula and needle technique to show where the hyaluronic acid is deposited and its proximity to the arteries. He reviewed the vascularisation of the specified area and the associated risks.