This content is limited to our registered members
-
Access exclusive business services unlimited
-
Access valuable features : audio listening & tools sharing with your patients
-
Access more than 150 product sheets, dedicated to professionals
You already have an account ? login now
BIODERMA Congress Reports RADLA 2022
Reports written by Dr. Silvina Maldonado (Dermatologist, Argentina) and Dr. Josefina Marco Bonnet (Dermatologist, France)
Related topics
Speakers: Dr. Ana Mordoh, Dr. Leonel Fierro, Dr. Francisco Bravo, Dr. Mario Marini, Dr. Miguel Martinez, Dr. Susana Puig, Dr. Raul Cabrara, Dr. Nelson Lobos and Dr. Carlos Silva
Report written by Dr. Silvina Maldonado
Genetic alterations in melanoma
Dr Ana Mordoh discussed genetic alterations in melanoma.
After reviewing the different types of genetic alterations (point mutations, indels, simplifications, deletions, gene misorderings, translocations), she mentioned that they are generally somatic, with 5% germinal alterations (familial melanoma). Some 94% of MMs have an altered RTK/RAS pathway (MAP kinases). As for the genetic classification of MM, she focused on BRAF, RAS, NF1 and TRIPLE WILD TYPE. The first three correspond to the MAP kinase pathway: BRAF, which is “druggable” with oncogene inhibitors, and “undruggable” RAS and NF1, the latter of which is insufficient to promote malignant tumour growth (playing only an accompanying role). TRIPLE WILD TYPE melanomas lack the signature of UV damage – these are the acral lentiginous / mucosal MMs with strong lymphocyte infiltration. In practical terms, patients with Intermittent Sun Damage (ISD), for which 30% of melanomas originate from a pre-existing naevus or melanocytes with BRAF mutations, are less than 55 years old, with many naevi located on the trunk and extremities, with BRAF predominance and low mutational load (TMB). In contrast, melanomas in patients with Chronic Sun Damage (CSD) originate from basal melanocytes or the follicular epithelium; these patients are less than 55 years old, with elastosis, actinic keratosis, few naevi on the head and neck or back of the hands, and high TMB, and are NRAS, NF1, KIT, BRAF.
Melanoma classifications
Dr Leonel Fierro reviewed melanoma classifications from a clinical perspective, and among the varieties, he discussed amelanotic spitzoid (favourable course in patients under 10 years of age) and mucosal melanomas (pagetoid, lentiginous or mixed patterns), as well as the malignant blue naevus type, which emerges from a cellular blue naevus or naevus of Ota and develops in the dermis and SCT without affecting the epidermis. With regard to special considerations for MM, he discussed MM in pregnancy (2.8 to 8.5% per 100,000, after neck and breast cancer); he presented an algorithm for surgical treatment (JDDG 2016 Jun; 14(6):585-93), but while he emphasised that pregnancy is not an indication for delaying treatment of MM, he also insisted on the importance of a multidisciplinary Bioethics Committee to make decisions in cases of metastasis. The rate of metastasis to the foetus is 25%, and the prognosis depends as always on the stage of disease progression. As for synchronous MM (multiple primary MM), it occurs when the diagnosis is made within the first 3 months of tumour development and there is a CDKN2A alteration in 8.3–15% of cases, with two age peaks: from 15–39 and from 65–79 years of age, mainly in the extremities, with a history of dysplastic naevi, family history of MM in first-degree relatives, light phototype. MM in children is rare, may be transplacental, via transformation of CMNs, associated with genetic conditions or on top of a pre-existing naevus.
Uncommon clinicopathological varieties
Dr Francisco Bravo reported on uncommon clinicopathological varieties.
Desmoplastic MM (4%), mostly in men older than 60, head and neck, non-specific clinical appearance, 60% amelanotic, de novo or associated with lentigo maligna, generally thick, but oddly enough less aggressive, better prognosis for pure type than mixed type. Primary dermal MM (0.8%), histologically indistinguishable from MTS, low metastatic potential, 80-100% survival at average Breslow thickness of 3 mm. Minimal deviation MM is equivalent to the vertical growth phase of MM but with no cytological atopy. Polypoid MM is a variant of nodular MM, not necessarily pigmented. May present in the upper respiratory tract, oesophagus, rectum, vagina, biliary tract, with no fixed genetic pattern, highly aggressive and generally in younger people aged 20 to 39. Verrucous MM (3%) often leads to diagnostic errors, in the legs and cheeks in young women and very aggressive if not in situ. Pigmented epithelioid melanocytoma (previously known as animal-type) has a low recurrence rate, low lymph node dissemination and systemic dissemination. 1/3 of cases are congenital or from childhood. Mucosal MM (1%) is frequently diagnosed late. Naevoid MM in young people, proximal areas of extremities and trunk, with frankly malignant behaviour. Large nested MM, generally in the sixth decade of life. Amelanotic MM: difficult to diagnose. Follicular MM, simulates itchiness in photoexposed areas. Rhinophymatous MM, difficult to diagnose. Wiesner naevus (BAPoma) is not an MM, but generally a syndrome marker with susceptibility to different types of cancer. Finally, Dr Bravo concluded his presentation with an extremely rare bilateral acral lentiginous melanoma with simultaneous presentation.
Recent changes to the T (TNM) and its utility in requests for studies and treatments
Dr Mario Marini presented recent changes to the T (TNM) and its utility in requests for studies and treatments.
He discussed the T’s importance in distinguishing clinicopathological variants of the primary tumour, physiopathology, and molecular studies. He noted that currently, only Breslow and ulceration remain in use for staging purposes (the other indices are optional, but must be reported if present in quantity). He mentioned the creation of subcategory T1b (between 0.8 and 1 mm) in determining whether or not to request a sentinel lymph node (SLN) study, based on the percentage of positive SLNs to avoid unnecessary biopsies. It should be considered in cases of T1a with ulceration, T1b with or without ulceration, and T1a with risk factors (young, high history index, lymphovascular invasion, >75% of HP regression or neurotropic type). This points to the importance of performing complementary studies according to staging, only in cases of advanced tumours and positive SLNs. Ultrasound is very useful for non-palpable lymph nodes and does not replace SLN. It should be requested if the patient meets the criteria for an SLN biopsy and does not have it done, if the SLN was not possible or was technically unsuccessful and when lymphadenectomy is not performed in the context of a positive SLN. At present, its use in Stage IV is being discussed in cases where lymphadenectomy or ultrasound monitoring is performed.
Requesting imaging and lab studies: when, and which ones?
Later, Dr Miguel Martinez talked about when to request imaging and lab studies and which ones to request.
In the diagnostic process, we must base our decisions on clinical observations, HP and potentially the emerging FISH molecular profile for diagnosis of ambiguous melanocytic lesions.
In the prognostic process, for initial staging and treatment planning, SLN biopsy is used after ultrasound of the lymphatic basin.
In the monitoring process, for diagnosis of recurrence or dissemination, in cases where it is determined that there is no additional benefit in low stages (up to IIA); in IIB and IIIA, IIC and IIIB, a cranial, thoracic and abdominal CT scan (and neck if indicated) should be requested, and in the latter two stages, PET-CT is an option, not examining the CNS without symptoms. In IIIC and IIID, CT scan of the entire body or PET-CT and brain NMR. If MTS is suspected or symptoms are present: PET, LDH and NMR.
Women with a history of melanoma (pregnancy, replacement therapy, etc.)
Dr Susana Puig discussed women with a history of melanoma (pregnancy, replacement therapy, etc.). She noted that the prognosis for MM does not change significantly during pregnancy and that this is the tumour that is most likely to metastasise to the placenta and potentially to the foetus, but that the development of both of these depends on the clinical stage of the disease. Regarding the risks of immunotherapy during pregnancy with PD1 inhibitors (nivolumab), there are some successful cases even though there is a risk of miscarriage up until week 14, and an increased risk in the second and third trimesters of foetal death, premature birth and infant mortality. Always analyse the placenta to assess the risk to the child. Regarding HRT, despite the fact that MM has estrogen receptors that can act as a stimulus to its growth and invasion, some studies have shown improved survival in women and that this therapy is safe.
Risk prediction in melanoma and the utility of molecular studies
Dr Raul Cabrara talked about risk prediction in melanoma and the utility of molecular studies. He noted that there are 20 genes associated with MM, some of them very frequent but low-risk and others which are rare but with moderate or high risk. For predicting the risk of hereditary MM, doctors can use INVITAE, preferably as a blood test but also via saliva, buccal smear, or DNA; for clinical risk of recurrence, MTS in melanomas treated via surgery, targeted therapy or immunotherapy, MELAGENIX can be used for biopsies, or SKYLINE (in development at the Mayo Clinic) or SIGNATERA as blood tests. They must be used with caution as they are currently being studied in anticipation of more precise information allowing for their universal use.
Surgical management of primary melanoma
Dr Nelson Lobos discussed surgical management of primary melanoma, placing a particular emphasis on fusiform excision or deep shave biopsies whenever possible with a minimal margin and for diagnosis with subsequent treatment measures; in the longitudinal direction in the extremities and otherwise following Langer lines, either with primary closure or healing by secondary intention; and in certain situations, multiple incision biopsies (on the face, with large lesion areas or low suspicion of MM). Margin extension is based on the Breslow depth (NCCN 02/2022). For special cases like subungual MM, there is no evidence that amputation yields even a modest increase in survival, and for lentigo maligna, first-line surgical treatment with monitoring of margins (wide excision, staged square or Mohs techniques if large in size, poorly defined or with microinvasion). Do not use electrosurgery.
Treatment of advanced melanoma: 2021 results
To conclude the session, Dr Carlos Silva discussed the treatment of advanced melanoma: 2021 results.
He presented a broad review of studies in which it was shown that a combination of BRAF and MEK inhibitors yields greater survival than use of either individually or placebo, except for Wild-Type BRAF for which equivalent results were observed with use of a combined regimen or nivolumab alone. In any case, there is no level I evidence (randomised phase III trials) to decide which treatment is the most appropriate for MM with BRAF mutations. Either choice is appropriate since they are based on evidence from clinical trials. There is no difference in overall survival. Targeted therapy is more effective in its response but more toxic (except nivolumab + ipilimumab), and requires ongoing treatment. It is still a matter of discussion whether to start early post-surgery therapy in Stage III, or to operate and provide treatment later when Stage IV is reached.
Speakers: Dr. Jose M. Mascaro and Dr. Arnaldo Aldama
Report written by Dr. Silvina Maldonado
Managing pemphigus vulgaris (PV) for the general dermatologist
For the specific topic, New developments in blistering diseases, Dr Jose M. Mascaro discussed managing pemphigus vulgaris (PV) for the general dermatologist.
Diagnosis is based on clinical signs, compatible HP, detection of IG (+/-C3) in intercellular spaces (ICSs) via IFD and of autoantibodies in the serum (IgG autoantibodies against ICS via IFI/ against Dsg3 (+/-Dsg1) via ELISA or other techniques). For treatment, two steps should be considered: the first aims to induce remission to achieve control of the disease and then consolidation, and the second aims to maintain remission. To accomplish this, rituximab (RTX) is considered to be the first- line treatment, for use in mild PV (<5% of body surface, does not affect ingestion of food, PDAI<15),
either alone (2 infusions of 1 g) or in combination with prednisone at lower doses than those that were used a few years ago (0.5 to 1 mg/kg/day with gradual reduction leading to suspension in 3-4 months). Prednisone 0.5-1.5mg/kg/day is also used alone or in combination with azathioprine, mycophenolate mofetil/mycophenolic acid. For moderate to severe PV, with difficulties ingesting food or >5% body surface and PDAI >15, rituximab is indicated at 2 infusions of 1g combined with prednisone 1mg/kg/day with gradual reduction leading to suspension in 6 months, and if this is contraindicated, the corticosteroid can be combined with AZT or MMF. If the disease is well controlled at 3-4 weeks, continue at the same dose and at 6 months, if complete remission (CR) has been achieved, rituximab is indicated at 500mg or 1 g if it was severe or if high levels of anti-Dsg antibodies persist at 3 months. If CR is not achieved, 2 infusions of 1 g of rituximab at 12 and 18 months, RTX 500mg in patients with CR if they continue to be positive for anti-Dsg antibodies. If the case is not under control at 3-4 weeks and the patient had already received prednisone and RTX, increase corticosteroid to 1.5mg/kg/day or IV pulses. If they had only received prednisone, increase dose and add RTX or immunosuppressants. First-line treatment with RTX increases the 5-year CR rate relative to second- and third-line use. It is worth noting that guidelines have not yet been established to avoid relapses, and proposals include systematic use at 6, 12 and 18 months (EADV Guidelines 202), retreatment with a large number of cycles, or personalised treatment based on biomarker evolution (anti-Dsg antibodies, CD20 lymphocytes, T cells).
Long-term management of pemphigus foliaceus with cortisone-sparing agents
To conclude the day, Dr Arnaldo Aldama discussed the long-term management of pemphigus foliaceus with cortisone-sparing agents. Corticosteroids can be used in oral or parenteral form, in a bolus, intralesionally and even topically, with daily or divided dose schedules or with alternating doses, at the lowest possible dose and in combination with other drugs to reduce their dosage and maintain remission. Options include AZT, MMF, RTX and potentially DAPS and cyclosporine. In severe cases, Ig 2-3g/kg on 4-5 days each month, plasmapheresis or immunoadsorption (eliminates 80% of circulating antibodies, in monthly cycles of 4-5 days, but only available to a small number of doctors). As topical treatments: clobetasol, topical ATB, tacrolimus. It is also recommended to take environmental, dietary and photoprotection factors into account.
Speakers: Dr. Graciela Guzman, Dr. Natalia Hernandez, Dr. Lucie Puell, Dr. Ida Duarte, Dr. Ana M. Gimenez and Dr. Juan Pedro Russo
Report written by Dr. Silvina Maldonado
Emerging allergens: old and new
Dr Graciela Guzman said that there are probably no new allergens, except perhaps substitutions by more allergenic molecules, since there is a lot we don’t know about nanotechnology and its toxicity. These allergens are found in everyday items for personal, work-related and recreational use, in medical equipment/implants, and recently we have especially seen allergens associated with personal protective items. In terms of sensitisation to metals, there seems to be a genetic predisposition with alterations to the filaggrin complex. Nickel is the number one allergen, often co-occurring with cobalt and chromium as well as palladium (combined in alloys for dental procedures). In addition to its presence in metals, it is found in diet due to pots that release it, but it also occurs in almonds, nuts, oats and cacao. It is highly prevalent in women – face, neck and hands. It is followed by perfumes and cosmetics (oxidised fragrances): magnolia officinalis, linalool and limonene, methyl glucose dioleate, and carbomers, but as the “allergen of the year”, she mentioned glycolipid and alykl glucosides, which are present e.g. in a commercial product, Tacrolimus (ELIDEL). In cheilitis, perineal dermatitis and stomatitis, the role of mint, cinnamal, anethole, propolis and metals. Dexpantelol (B5) in moisturisers and cosmetics. In stomas, N-butyl monoester of polymethyl vinyl as well as isobornyl acrylate in glucose monitors.
Contact dermatitis: experience in a dermatological unit
Dr Natalia Hernandez presented a 5-year project in which 64.7% of patients had positive tests on the European standard series, with reactions caused by nickel, fragrance mix I, Peru balsam, fragrance mix II, and methylisothiazolinone (the latter is present in the “slimes” that children play with). She presented clinical cases in which the substances triggered contact dermatitis in different parts of the body, and in which it was not always easy to determine the mechanism by which the contactant produced the reaction. She noted the frequency of allergen positivity in atopic patients and the impact on their quality of life.
Common allergens identified by patch tests in patients with suspected contact dermatitis of the face
Dr Lucie Puell discussed patterns for guiding clinical suspicion: bilateral patchiness, which affects the forehead, cheekbones and chin; airborne, in which the neck is added but the nose is spared; and photoallergic, in which the nose is affected in addition to all of the above. Of the 1800 children and adolescents who were studied, about 70% were female, most with reactions on the face and hands. Reactions were noted on the face for wool alcohols, nickel, and potassium dichromate, and on the hands for nickel/cobalt/potassium dichromate and wool alcohols, in order of frequency. In another study in adults, the frequency was very high on the hands and less on the face/rest of the body, with nickel, cobalt, fragrance mix and chromium being the most commonly involved. She also emphasised the importance of ruling out associated pathologies and two forms together like the occupational and non-occupational airborne forms. Healthcare personnel have been affected by rubber accelerators in elastic bands on masks, formaldehyde, and adhesives like dibromodicyanobutane.
Metallic implants and hypersensitivity reactions
Dr Ida Duarte talked about metallic implants, especially trauma implants since those are the ones for which the most data are available, but also extending the discussion to other types (gynaecological
implants, pacemakers, intravascular and dental implants), and to the dilemma as to whether the failure of an implant is due to a hypersensitivity reaction or vice versa… These reactions manifest as erythema, eczema, oedema and/or joint pain, and present 2 months to 2 years after surgery, with greater frequency in women. The Major Criteria are: onset of chronic dermatitis weeks to months after implantation, positive contact tests for implant components, and complete resolution after implant extraction. The Minor Criteria are: treatment-resistant dermatitis, systemic ACD (allergic contact dermatitis) reaction, ACD physiopathology, and a positive lymphocyte transformation test for metal.
She noted that the sensitisers are nickel (20% sensitisation), chromium (10%) and cobalt (10%), and that these are found in almost all metal alloys:
- stainless steel (19% Cr, 9-33% Ni as well as molybdenum, carbon and nitrogen),
- Co-Cro-Mo (67% Cr, 30% Co, 2% Mo and 1% Ni),
- titanium alloys (91% Ti, 5% Al, 3.9% vanadium and 0.1% Ni).
Other components: methacrylate, benzoyl peroxide, N,N-dimethyl 4 toluidine (accelerator), gentamicin and hydroquinone. Familiarity with these factors is essential in determining the approach to be taken. A study was conducted with 72 patients in which pre-surgical tests were performed only if they had a prior history of allergy to metals (31 tested and 21 positive results, for whom a prosthesis was selected in accordance with the results); the other 41 were tested for post-surgical symptoms and only 10 were positive, of whom 6 had the implant removed with subsequent improvement; the remaining 4 refused. It’s very important to make clear that the pre-operative test indicates a current allergen and does not predict a future allergy, and that a positive post-operative test does not necessarily indicate that the ACD is responsible for the implant’s failure. If it is not possible to remove the implant, systemic corticosteroids are indicated for 21 days; in many cases, adaptive biological immune tolerance is achieved in this time.
Listening to patients: lessons learned in a centre for the study of contact dermatitis
Dr Ana M. Gimenez discussed the difficulty often encountered in objectively verifying the cause of ACD, since the standard tests often do not include the components that emerge from detailed questioning of the patient, and presented clinical cases in which a bit of detective work revealed the source of the reaction. Among others, she presented a case in which the difumarate found in the desiccant packets located in sofas and footwear from China triggered an epidemic in Europe, which led to a request for trade restrictions. Another interesting case was positive 2,4-dichlorophenol, found in bikinis, which caused urticaria reactions. She mentioned the reactions following administration of Moderna and Pfizer vaccines (mRNA), especially “covid arm”, which yield negative results for patch tests but positive results in intradermal reaction tests for polyethylene glycol. In conclusion, she presented the case of Myolastan (tetrazepam), which had to be taken off the market following severe illness among machine maintenance staff due to aerial suspension of the product.
Prevention of occupational dermatoses for healthcare personnel in the time of the covid-19 pandemic
Dr Juan Pedro Russo presented the consequences of the use of PPE (personal protective equipment) and recommended identifying areas of increased pressure if pain or non-blanching rash appears in order to avoid pressure lesions; removing after 4 hours; applying a moisturiser or silicone-based cream an hour before; and in case of a non-blanching rash, applying a hydrocolloid bandage. To avoid aggravating rosacea: skin cleansing, barrier restoration using non-sensitising products without fragrances or preservatives, examination and treatment of vascular reactivity, and examination of inflammatory response. Also for dermatitis of the hands, avoid very hot water, opt for glycerine-rich hand sanitisers, emollient-rich and preservative-free moisturisers, and vinyl/nitrite gloves.
Speakers: Dr. Phillip Tschandl
Report written by Dr. Silvina Maldonado
Dr Phillip Tschandl led an interesting plenary session on the pros and cons of artificial intelligence (AI) in dermatology. He presented different studies which ultimately showed that existing algorithms can be of great assistance, especially in the education of young doctors, but that when projected to use by the general population, they only generate false positives and high anxiety among patients, further increasing the cost of healthcare. “Machines only see what they know,” so they can only produce diagnoses based on the data in their systems. Use of AI for dermatoscopy using home devices is not useful if the at-home patient does not take the photo of the lesion correctly and the diagnosis is lost, making it useful for an experienced dermatologist but not for the patient. A German study showed that when using AI as a second opinion in comparison with a diagnosis by experienced dermatologists, the data matched, making it very useful for malignant cases. The future looks very promising for follow-up images and full-body mapping, as well as confocal microscopy. In conclusion, it is clear that Artificial Intelligence will make our lives easier, but there are not yet any prospective studies that prove the benefit. On a final note, he invited the audience to learn more about DERMONAUT.
Speakers: Dr. Agustina Zambernardi, Dr. Vania Diaz Perez, Dr. Ianina Massimo, Dr. Ana Buongermini, Dr. Claudia Suarez and Dr. Cristina Carrera
Report written by Dr. Silvina Maldonado
Approaches for patients with suspected pharmacodermia
The speaker presented a brief review of pharmacodermias, referring to them as “another big simulator” due to the large number of patterns, then discussed a practical treatment strategy, and finally talked about the tools currently in use and in development. The predominant lesion type is important to the strategy in terms of how we think about the pathophysiology, since urticaria will point us to an immediate reaction to preformed mediators (exposure in the previous 6 hours) whereas maculopapular exanthema/SDRIFE (symmetrical drug-related intertriginous and flexural exanthema)/bull’s eye rash/petechiae suggest delayed action (more than 3 days). She presented various clinical cases with the steps taken up to identification of the suspicion and diagnostic confirmation, always assessing the severity and acting on suspicions without waiting for confirmation. As for whether it is worthwhile to try and identify the trigger, given that these patients are often polymedicated, she suggested waiting 4-6 weeks after complete resolution and only in cases where doubt remains, where there is no equally effective alternative, and where the risk/benefit ratio is favourable since the patient has to go without medication. The tools in development are prognostic and diagnostic genomic biomarkers. HLAs have the disadvantage of not being extrapolable to the entire population, Circulating Proteins and PCR are non-specific, and others are being studied.
DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms)
Dr Vania Diaz Perez discussed DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms), potentially fatal and with skin and visceral involvement. Regarding its pathogenesis, she talked about its relationship at the onset to specific drugs, incomplete drug metabolism with accumulation of reactive metabolites, and reactivation of herpes viruses, especially HHV6, the presence of which is not essential but seems to be an aggravating factor resulting in a prolonged and fluctuating case.
There appears to be a genetic predisposition, with mutations in genes that code for drug metabolising enzymes (like cytochrome P450 and N-acetyltransferase), and as a result, accumulation of the drug or its toxic metabolites interacts with cellular peptides or proteins to provoke immune responses and hypersensitivity reactions. Among the drugs involved, she mentioned anticonvulsives, ATB, antiretrovirals and analgesics/antipyretics. She emphasised the issues of late onset (3 weeks after starting the drug), a prolonged course of up to 1 year in some cases, and a longer latency period than SJS/TEN/AGEP, fixed drug eruption and exanthematous maculopapular drug eruption. The risk factors for a prolonged clinical course are high levels of basal lymphocytes and liver enzymes, and reactivation of various HHVs. Recurrences are usually milder and may also be due to a structurally unrelated drug, although the mechanism is unknown. For Diagnostic Criteria, she mentioned RegiSCAR and DiHS, emphasising that they are essentially equivalent but that the latter includes HHV6; for the prognosis, she noted a mortality rate of 10%, comorbidities and autoimmune diseases in patients who recover from DRESS at 1-2 months after recovery, with a likely connection to HHV6 reactivation. With regard to histopathology, she mentioned different non-specific patterns, but 50-60% of cases show 2 or more of these patterns coexisting. Treatment consists of immediate cessation of the drug, use of systemic corticosteroids (despite its complications, it is still the main tool), and although there is no consensus about the severity for which it is indicated, it is recommended when transaminase levels are elevated by a factor of 5 or when other organs are affected. Supportive care, IgIV, immunosuppressants and ganciclovir should also be considered.
Toxic epidermal necrolysis (TEN)
Dr Massimo presented various clinical cases, particularly that of a boy who developed DRESS from an anticonvulsive drug with good response to treatment; later, however, in continuing to administer the drug, his mother developed a case of TEN that lead to her death. She emphasised the importance of early treatment in the ICU, appropriate personnel, the importance of the patient’s previous state of health, prompt cessation of the drug in question, recovery and support, and vigilance against infections.
Childhood pharmacodermias: clinical cases
ADRs are a very common part of daily paediatric practice, and the skin is the affected organ in 35% of cases. Most are mild and resolve with cessation of the drug, but severe cases are also encountered. There are distinct physiopathological mechanisms and morphological manifestations, with exanthemas being the most common form of presentation, and this represents a diagnostic challenge in children since they can imitate other rashes commonly seen in this stage of life, making the dermatologist’s role a very important one.
Advances in the investigation of severe adverse drug reactions of the skin
Dr Claudia Suarez talked about advances in the investigation of severe cutaneous adverse drug reactions, specifically SJS/TEN; the pathogenesis of these reactions has not yet been completely explained, but it appears to be a specific cytotoxic T CD8+ response in the context of MHC class I. This causes massive apoptosis and necrosis of keratinocytes, low cytotoxic lymphocyte counts in the skin, and presence of measurable soluble mediators (biomarkers). The biomarkers that generate APOPTOSIS are:
- Soluble FAS ligand, with early increase and rapid decline (does not increase in common ADRs).
- Perforin and granzyme B (reliable markers of SJS/TEN), early increase in serum/blisters and association with severity of skin ADR; its inhibition attenuates lymphocytes’ cytotoxic effect in TEN blisters and is therefore a potential therapeutic target.
- Granulysin, early expression and rapid decline; its plasma and blister level is correlated with severity and has been associated with acute ocular involvement. It allows for a rapid chromatography test and is therefore more convenient.
- The role of micro RNA (miRNA) is unclear.
- Galectin has a pro and anti-apoptotic role, increases in serum in SJS/TEN, decreases with treatment of the disease and therefore measures activity, but it is non-specific.
The biomarkers that generate NECROPTOSIS are: Annexin A1, a possible therapeutic target, and RIP3 associated with activity, severity, and allows for monitoring of the response to treatment. Other cyotkines and biomarkers: HMCB1, IL15 (prognostic factor and potential therapeutic target), IL13, IL6, TNF alpha, IP10 and S100A2. In conclusion, biomarkers help us to understand physiopathology and are useful for early diagnosis, determining severity, response to treatment and phenotype; they will also help to develop new treatments, with the possibility that they will need to be used in combination.
What dermatologists need to know about adverse reactions to new cancer immunotherapy treatments
Cancer immunotherapy unblocks immunotolerance, leading to activation of various “-itis” disorders. In the US alone, 50% of people with cancer of various types will receive immunotherapy. A study shows that 50% of patients with melanoma (MM) will present global toxicity (average 125 days) in the gastrointestinal tract earlier on, and in the skin, hepatobiliary and other systems, which is maintained over time. Immune-mediated adverse effects can appear at any time, even after the drug has been suspended. The skin is the most frequently affected organ, which is why we need to recognise these adverse reactions. Dr Carrera presented cases of morbilliform exanthema/spongiotic dermatitis, autoimmune diseases of connective tissue (DM, SLE, SJS, …), vitiligo-like depigmentation, lichen planus-like eruptions, psoriasis rupioides, autoimmune blistering dermatoses induced by PD1 inhibitors, sarcoidosis reactions. She raised the possibility that adverse effects are markers of a better prognosis, though not in the intense forms, which are more serious.
Speakers: Dr. Cristina Santana, Dr. Roberto Alas, Dr. Luisa Gonzalez and Dr. Emerson Andrade
Report written by Dr. Silvina Maldonado
The different faces of scars
Dr Cristina Santana talked about the different faces of scars, starting with a clinical review of the various types. She recommended respecting the tension lines on the body, monitoring the tension lines from the start, and informing the patient about therapeutic options.
Traditional approaches to scar treatment
Dr Roberto Alas discussed traditional approaches to scar treatment. In terms of prevention, decide on the right incision technique to reduce skin tension by following relaxed skin tension lines, and the appropriate suturing technique. With a small keloid scar, use infiltrations or pressure therapy after removal, and if it is large, then adjuvants. Botulinum toxin has been shown to be effective in inhibiting scar hyperplasia when applied immediately after suturing (3-5 U), thus improving its appearance. For at-home management, he suggests using silicone bands. For scar correction procedures, he mentioned the traditional use of TCA, 5-FU, TGF-beta3, cryotherapy, fractionated CO2 lasers and 532/1064 nm picolasers; Tixel (thermomechanical ablation), microneedling (electromechanical) and laser-assisted drug delivery. He showed the use of infiltration with a mixture of TAC 40% (1/3), Meso CIT K (1/3) which is an FTBeta 3, TGFBeta/SMA pathway inhibitor, and lidocaine 2% (1/3). Another mixture combines half ivermectin 1% (fibroblast inhibitor) and half lidocaine 2%, which allows for the procedure to be repeated and with no associated neurotoxicity; he noted that he uses the drug for veterinary use due to the unavailability of the injectable drug in his country. He concluded by stating that a combination of therapies/procedures is the best option.
Hard-to-treat scars
Dr Luisa Gonzalez talked about hard-to-treat scars with a review of clinical cases.
Percutaneous Collagen Induction with Needles (IPCA)
Dr Emerson Andrade discussed Percutaneous Collagen Induction with Needles (IPCA), which causes platelets and erythrocytes to be released, thereby releasing TGFalpha1, TGFbeta3, PDGF, FGF and VEGF. Petechiae/purpura formation occurs, with chemotaxis in minutes to days and invasion of inflammatory cells. It is indicated for flaccidity, hyperpigmented scars, acne scars, traumatic tattoos, melasma (increase in keratinocyte replication kinetics) with the LIMA protocol: anaesthesia with liposomal lidocaine 1 hour before, moderate injury from 1.5 mm needle depth with diffuse erythema at 30-day intervals, minimum 2x and resume depigmentation treatment at 24 hrs. He also discussed a subcision technique (dermal tunnelling) for acne scars and other depressions, as well as for deep wrinkles that cannot be helped using fillers, which can be combined with IPCA. He presented cases in which deep needling was performed post phenol 88%. Finally, he discussed the use of FRAXX with multineedling for submental retractile injury, eyelid pigmentation and flaccidity, wrinkles on the chest, and dystrophic post-graft scars.
Speakers: Dr. Claudia Marchitelli, Dr. Juana Benedetto and Dr. Mirtha Cifuentes
Report written by Dr. Josefina Marco Bonnet
Vulvar Intraepithelial Neoplasia (VIN)
There are two groups of VIN.
1. Related to HPV: classic VIN
a- Low-grade squamous intraepithelial lesion (LSIL)
- No treatment since there is no risk of degeneration. It can even spontaneously disappear within two to three years.
b- High-grade squamous intraepithelial lesion (HSIL)
- More common, often affects young people
- Multifocal, with lesions that may be greyish, red, white or pinkish and can affect the vulva, perineum, vagina, cervix and anus
- The vulvar anatomy is respected
- Has a good prognosis, so conservative treatments should be favoured (imiquimod, CO2 laser). Imiquimod (three times a week) can be used for 16 weeks or more, until the lesions disappear
2- Related to lichen sclerosus (LS): differentiated VIN
- In older patients
- Unifocal, white
- The vulvar anatomy is altered
- It is the precursor of vulvar carcinoma (which develops within around two years)
- It is treated via surgery (5 mm margin) followed by clinical monitoring every six months for a period of five years. If LS is treated, the risk of differentiated VIN developing is reduced
Oral manifestations of autoimmune diseases
Desquamative gingivitis
- Mild gingival oedema and erythema
- Aggravated by a decrease in oral hygiene due to pain (increase in dental plaque, increase in inflammatory mediators such as TNF-alpha, IL-1, worsening of the disease)
- A distinction should be made between
1- Intermittent DG
- Erythema multiforme (erythematous, erosive, ulcerated lesions, with irregular borders, over the entire oral mucosa), of infectious origin (90%) or induced by medication
- Contact stomatitis (localised, keratinised, erosive, lichenoid lesions)
2- Persistent DG, caused by inflammatory and autoimmune diseases
- Erosive lichen planus
- Pemphigus vulgaris: mucosal lesions are the first to appear and disappear. They are caused by desmoglein 3
- Paraneoplastic pemphigus: the damage to the oral mucosa is more severe. It is associated with antibodies to envoplakin, periplakin and alpha-2-macroglobulin-like-1. It is necessary to test for non-Hodgkin’s lymphoma (42%), CLL (29%), Castleman disease (10%) and adenocarcinoma. For 10%, no cancer is found at the time of diagnosis.
- Mucous membrane pemphigoid: 85% oral involvement
- Acquired epidermolysis bullosa (anti-collagen VII antibodies)
- GvHD
- Linear IgA bullous dermatosis
Biopsies need to be performed with DIF, IDIF and ELISA for bullous diseases.
Allergic contact stomatitis
1- When should contact stomatitis be considered?
- If there are lichenoid lesions or stomatitis lesions resistant to treatment. If the lesion is unilateral. If there is a history of allergy.
- If there is an anatomical relationship between the lesions and the suspect material (direct contact or less than one centimetre).
- If the symptoms are chronologically associated with exposure to the allergen.
2- What to do
- Perform an elimination and reintroduction test
- No biopsy
- Perform patch tests, RASTs
3- The most common allergens
- Metals contained in appliances, amalgam: mercury, nickel, copper, zinc, chromium, cobalt, gold, silver
- Preservatives (sodium benzoate, propylene glycol, parabens, formaldehyde), antiseptics (chlorhexidine, triclosan, hydrogen peroxide), detergents (sodium lauryl sulfate), and whiteners contained in toothpastes and mouthwashes
4- Treatment
- Avoidance of the allergen. This is not always easy; we need to work with dentist teams. The lesions disappear in 37 to 100% of cases.
- Locally, we can propose topical corticosteroids and topical tacrolimus.
Speakers: Dr. Meire Parada, Dr. Vanessa Piquero
Report written by Dr. Josefina Marco Bonnet
Late complications of hyaluronic acid (HA)
This type of complication occurs more than 30 days after the HA injection.
It can take the form of oedema, inflammatory nodules, non-inflammatory nodules, infections, granulomas and biofilms.
- Oedema caused by lymphatic obstruction.
This is an early, painless type of oedema that usually affects the malar region following tear trough filler injections (around 2%). To avoid it, we should question our patients and not perform injections in this area in female patients who have eyelid oedema when getting up in the morning.
- Intermittent and persistent delayed-onset oedema.
This is a delayed-onset, inflammatory type of oedema that affects the lower eyelids and the malar region and occurs in the morning. There are no palpable nodules. Ultrasound shows features of panniculitis.
We need to investigate triggering factors such as flu-like syndrome, an upper airway or sinus infection, a dental infection, trauma, COVID infection, or COVID vaccination.
Treatment involves a sometimes ultrasound-guided hyaluronidase injection.
- Non-inflammatory nodules are usually due to the accumulation of HA. Treatment consists of massages and hyaluronidase injection with a needle or cannula.
- Inflammatory nodules are of infectious origin.
- If they are small, we propose antibiotic treatment (clarithromycin 500 mg twice/day or doxycycline 100 mg twice/day or clindamycin 600 mg) and we re-evaluate the patient after 48 hours.
- Fluctuant nodules should be drained and the product obtained should be cultured to have an antibiogram. Pending the results, we should initiate probabilistic antibiotic therapy as seen earlier. If this is not sufficient, we can add hyaluronidase in a second phase.
- Fixed inflammatory nodules should benefit from an ultrasound +/- needle aspiration or an incisional biopsy if possible or a 4 mm punch biopsy. Biopsy will help identify the responsible product and determine if there is a granulomatous reaction, an allergic process, an infection or a biofilm.
Treatment combines antibiotics, hyaluronidase, oral or intra-lesional (IL) corticosteroids, 5FU (IL) and surgery.
- Inflammatory nodules and biofilms should be treated with clarithromycin 500 mg twice/day or doxycycline 100 mg twice/day for 10 days. If this is insufficient, treatment with ciprofloxacin (500 mg twice/day) or moxifloxacin (400 mg/day) can be proposed.
- Granulomas.
A biopsy is always necessary since the diagnosis is histological. Treatment involves oral (0.5 to 1 mg/kg/day) or IL (5-10 mg/cc) corticosteroid therapy or the combination of IL 5FU + corticosteroids (5FU 50 mg/ml 0.5 ml + triamcinolone 10 mg/ml 0.3 ml + lidocaine 0.2 ml).
Autoimmune diseases and fillers
There are not a lot of data. Caution is required.
The patient should be informed orally and provide their consent regarding the immunological risks of filler injections with vaccines, COVID and autoimmune diseases.
It is necessary to identify patients with a risk of developing an autoimmune/inflammatory syndrome
induced by adjuvants (ASIA) or delayed-onset inflammatory reactions, through interviews, biological tests and, in the future, HLA typing. ASIA syndrome is triggered in genetically predisposed patients (HLA B8 or DRB1). In these patients, biomaterials can cause a late immune response or even granulomatous or autoimmune reactions. It is aggravated by local traumas, infections, vaccines, dental amalgam and menstruation.
In at-risk patients, lisinopril (an ACE inhibitor) has shown to be effective by reducing the risk of late reactions. It can therefore be proposed prior to vaccination for these patients.
For these patients, fillers should be injected with a cannula, with small amounts of high-molecular- weight HA (less immunogenic).
The autoimmune disease should be inactive without treatment. Intradermal skin tests are feasible but the results should be read again after one and three months.
We think it is necessary to wait two to four weeks between HA injections and COVID vaccination. If the patient is at greater risk of inflammatory reactions, the waiting period should be longer (four to eight weeks). The treatment of complications is the same as for non-COVID causes.
Speaker: Dr. Bertrand Richert
Report written by Dr. Josefina Marco Bonnet
This is a dystrophic disorder of the great toenail (GT); it is present at birth and worsens during the first year of life. The nail has a triangular, hyperkeratotic, greenish appearance with multiple transverse grooves. This condition is painless.
Girls seem more often affected than boys and the most affected nail is the right GT. What to do:
- Monitor children with photos over a five-year period.
- Reassure parents, as it often spontaneously disappears.
- If there is no improvement after five years, surgery should be proposed. There is a 90% success rate, regardless of the degree of deviation and the patient's age at the time of surgery.
- Inform the parents that there is a 10% non-response rate with surgery. No explanatory factors for non-response have been identified. It seems that boys are better responders.
Speakers: Dr. Maria Teresa Molina and Dr. Andrea Santos Muñoz
Report written by Dr. Josefina Marco Bonnet
Diet and acne
Acne is a multifactorial disease. The Western diet is an aggravating factor for some of our patients. An overall management approach is necessary.
At a pathophysiological level, two factors explain the impact of diet on our skin: FoxO1 (forkhead box class O transcription factor) and mTORC1 (mammalian target of rapamycin complex 1). FoxO1 controls the signalling pathway of mTORC1.
FoxO1 is found in the sebaceous glands; it acts on immunity, cellular proliferation, apoptosis, lipogenesis, inflammation and antioxidant defences.
mTORC1 stimulates cellular proliferation and differentiation, sebaceous gland hyperplasia and sebaceous lipogenesis and promotes sebum production. It plays a major role in premature ageing and all civilisational diseases (acne, obesity, insulin resistance, type 2 diabetes, Alzheimer's disease and cancer).
The Western diet stimulates growth factors such as IGF-1 (insulin-like growth factor 1), the supply of cell energy (glucose), amino acids (leucine), glutamine and saturated fatty acids (palmitic acid). These factors stimulate the mTORC1 pathway.
Three families of foods reduce the activity of FoxO1 and activate the mTORC1 pathway. These are:
- high-glycaemic carbohydrates milk and dairy products
- saturated fat.
Some studies seem to show that patients with severe acne have levels of vitamin D below those of the control group. Vitamin D plays a role in regulating the innate and acquired immune systems and also in sebocyte and keratinocyte proliferation. It also has an anticomedonal and antioxidant effect.
Prebiotics are non-digestible dietary substances that generally contain carbohydrates known as short- chain polysaccharides and oligosaccharides. They ferment in the digestive tract and provide nutrients to the intestinal microbiome. Foods high in prebiotics include tomatoes, artichokes, onions, garlic, rocket, leeks, asparagus, berries, bananas, oats and pulses.
Probiotics may also have a role to play, but for the moment the studies undertaken have been insufficient.
In short
- Have balanced calorie intakes
- Avoid refined carbohydrates
- 3- Avoid intakes of leucine (milk and meat) and glutamine (milk)
- 4- Avoid processed foods (saturated fat)
- Stop taking food complements containing milk protein (whey)
- Eat vegetables, pulses and fruit with a low glycaemic index and fish high in omega-3 fatty acids
- Consume natural mTORC inhibitors (green tea, turmeric, soya, berries)
- Consume natural probiotics (sourdough bread, bitter cocoa, apple cider vinegar, miso, kimchi, sauerkraut, kombucha)
- In the event of severe or resistant acne, measure vitamin D levels
Cutaneous microbiome and acne
The microbiome is an ecosystem of invisible organisms that live in symbiosis with us. There are four microbiomes: gastrointestinal, pulmonary, urogenital and cutaneous. Each microbiome is unique, like our fingerprints.
The cutaneous microbiome is made up of 1 million bacteria per square centimetre of skin. There are 10 times more bacteria than cells and more than 1000 bacterial species that encode 150 times more genes than the human genome. Its roles include regulating the immune response and providing protection against pathogenic bacteria. The microbiome is influenced by intrinsic (genetic) and extrinsic (diet, living environment, cosmetics, sun, etc.) factors. The intestinal microbiome can also influence skin diseases by sending inflammatory signals through the bloodstream.
With acne, the following anomalies of the cutaneous microbiome are observed:
- The transformation of type II and III Cutibacterium (C.) acnes (healthy skin) into type I C. acnes which stimulates the Th1 and Th17 pathways.
- Staphylococcus epidermidis decreases, which increases the C. acnes biofilm. Therefore, C. acnes is more virulent and more resistant to antibiotics and shows increased survival.
- Malassezia is suspected of playing a role in resistant acne.
What should you do?
- Improve your diet to have a non-inflammatory digestive microbiome (see diet and acne).
- Avoid using topical antibiotics so as to not destroy C. acnes and to prevent biofilm formation. Use oral antibiotics as little as possible.
Speaker: Dr. Aimilios Lallas
Report written by Dr. Josefina Marco Bonnet
The evaluation of pigmented facial lesions using dermoscopy (DSC) is difficult, especially in cases of early-stage melanoma. Indeed, the presence of lesions without pigmented or bluish structures is a sign of invasive melanoma, which is often clinically diagnosed.
Dr Lallas proposes a reverse algorithm. If there are not any of the six dermoscopic signs of benign lesions, biopsy is necessary to rule out incipient melanoma. These structures should be located mainly on the lesion.
The DSC signs are:
- Scales: a sign of actinic keratosis.
- White and wide follicles or rosettes: a sign of actinic keratosis.
- Erythema or tree-like blood vessels: a sign of actinic keratosis.
- Branched or parallel lines (fingerprint-like): a sign of seborrhoeic keratosis (SK) or lentigo.
- A clear border: a sign of SK or lentigo.
- Conventional criteria for SK (globules, etc.).
This method was tested, with humans versus artificial intelligence, and humans won. The only limit to this algorithm: lichenoid keratosis.
The issue of overdiagnosis can be raised. However, an early diagnosis ensures easier and faster management, with less scarring for our patients.
Speaker: Prof. Henry Lim
Report written by Dr. Josefina Marco Bonnet
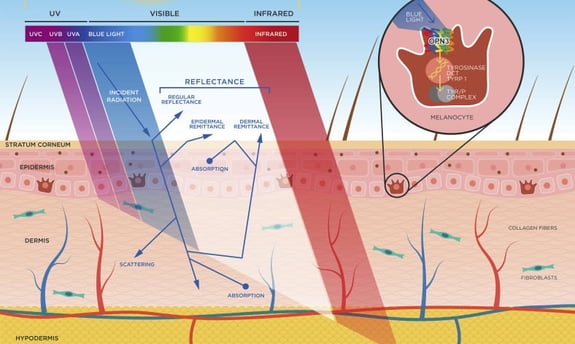
The spectrum of sunlight that reaches the Earth’s surface ranges from UV to infrared (IR) radiation. The closer the sun’s rays get to IR on the spectrum, the more deeply they penetrate the skin (see photo). The effects of these rays differ depending on the phototype and some have synergistic effects (VL and IR, and VL and UVA).
Photoprotection of the Skin from Visible Light‒Induced Pigmentation: Current Testing Methods and Proposed Harmonization
Henry W.Lim, Indermeet Kohli, Corinne Granger, Carles Trullàs, Jaime Piquero-Casals, Mridvika Narda, Philippe Masson, Jean Krutmann, Thierry Passeron
Journal of Investigative Dermatology Volume 141, Issue 11, November 2021, Pages 2569-2576
The photobiological effects of sunlight are:
Violet and blue light (BL) is responsible for the effects of VL. It stimulates the OPSIN 3 melanocyte receptor, which stimulates tyrosinase and causes the skin to become pigmented. UVA 1 has a synergistic effect with BL. They induce rapid and long-lasting pigmentation in phototypes III to VI. From a dermatological standpoint, VL contributes to the appearance of:
- Melasma and post-inflammatory hyperpigmentation (PIHP) in dark phototypes
- Erythema in light phototypes
- Photodermatoses (solar urticaria, cutaneous porphyria (PCT and EPP))
VL induces reactive oxygen species (ROS) in the skin and therefore contributes to skin ageing. BL from electronic devices does not induce skin pigmentation.
Speakers: Dr. Jaime Piquero and Dr. Ninosthka Guillen
Report written by Dr. Josefina Marco Bonnet
Photoprotection and hyperpigmentation
Dark-phototype patients are more likely to experience pigmentation disorders since their melanosomes are more labile and do not degrade melanin as well.
Five pathophysiological mechanisms have been described as being involved in melasma:
- Abnormal melanocyte activation
- Aggregation of melanin and melanosomes in the epidermis and dermis
- Increased number of mast cells
- Presence of solar elastosis and alteration of the basement membrane
- Increase in vascularisation.
BL and UVA 1 play a major role in melasma.
The ideal sun care product for dark skin:
- Would have a water-based formula (more cosmetic and pleasant)
- Would not leave white marks on the skin
- Would have a broad spectrum, with a high UVA protection index, SPF 30, active against VL
- Would have antioxidants to reduce ROS
- Would be tinted (primarily iron oxide) to protect against VL and conceal lesions
- Could contain depigmenting agents (niacinamide, resorcinol derivatives, etc.).
A sun care product providing protection against UVB rays, short- and long-wave UVA rays and VL is therefore necessary. Here are the six key points to keep in mind when choosing your sun care product:
- There are few filters covering long-wave UVAs (>400 nm): Mexoryl 400 and TriAsorB.
- To protect yourself from VL, you need a tinted sun care product containing iron oxide, zinc oxide or titanium dioxide. This poses compliance problems, since tinted products are not suited to all skin tones; they can also be thick and can stain clothes. There is no label indicating the degree of protection against BL. The following link gives a list of sunscreens that protect against BL; it includes information about the available shades (universal, light or dark) and the SPF, price, and other characteristics: http://dx.doi.org/10.17632/dtb4y9b684.
- You need a sun product with antioxidants such as niacinamide, licochalcone A, beta-carotene, vitamins E & C, glycyrrhetinic acid or diethylhexyl syringylidene malonate (DESM).
- You should consider an oral photoprotection product such as Polypodium leucotomos extract (PLE), which improves protection against VL.
- We need to educate ALL our patients about photoprotection, from the lightest- to the darkest- skinned individuals.
- We should adapt our advice concerning photoprotection products based on the phototype.
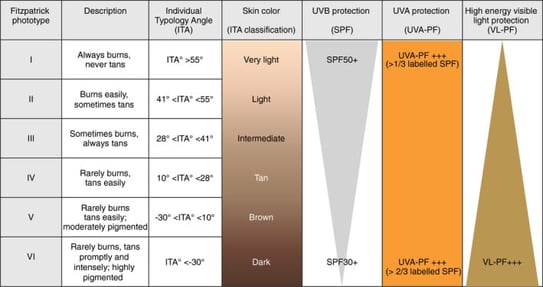
Phototypes I to III require an SPF 50, UVA 1/3 protection, and a low level of BL protection. On the other hand, phototypes IV to VI need a lower SPF (30) and UVA 2/3 (mainly long-wave) and BL protection.
Photoprotection according to skin phototype and dermatoses: practical recommendations from an expert panel
T. Passeron, H.W. Lim, C.‐L. Goh, H.Y. Kang, F. Ly, A. Morita, J. Ocampo Candiani, S. Puig, S. Schalka, L. Wei, B. Dréno and J. Krutmann J Eur Acad Dermatol Venereol. 2021 Jul; 35(7): 1460–1469
Photoprotection of difficult areas: eyes and lips
Three important points:
- For the eyes, the sun should be avoided from 8 to 10 am and from 2 to 4 pm. The sun’s rays are parallel to the eyes and are therefore more harmful.
- Sunglasses should be purchased from an optician because others can dilate the pupils, allowing more UV rays to pass through.
- Photoprotection should be applied to the lips six times a day.
Speaker: Dr. Esther Freeman
Report written by Dr. Josefina Marco Bonnet
Several points struck me as important.
- The most vaccine-specific skin reaction is the appearance of an inflammatory plaque on the injection site after seven to eight days. It disappears spontaneously within a few days. It may reappear following a booster dose but occurs more rapidly (D2-D3) and also disappears more quickly. It is a delayed hypersensitivity reaction and we do not know what patients are reacting to.
- There have not been any cases of anaphylactic shock.
- Skin reactions have been more frequent with Moderna.
- Forty-three percent of patients who have had a cutaneous adverse effect following the first dose experienced recurrences with booster doses. The recurrences were earlier and not as severe.
- There have been post-vaccination COVID toes (frostbite-like rashes).
- Bullous eruptions have been described, including biologically and histologically confirmed bullous pemphigoid (BP). Two sub-groups of BP patients have been observed.
- Older patients with BP that progressed as usual. It is thought that the vaccine revealed underlying BP.
- Younger patients with BP that disappeared rapidly and spontaneously.
Speaker: Dr. Justin Endo
Report written by Dr. Josefina Marco Bonnet
Pruritus is a very common symptom, with 78% of individuals over the age of 65 complaining of it. It impacts quality of life, is associated with depression, disrupts sleep and reduces productivity. The pathophysiology of pruritus is complicated.
The BINDIS acronym summarises why older patients feel a need to scratch:
- Barrier function decline
- Immunosenescence: the Th2>Th1 pathway
- Neurological. It may be due to central or peripheral neuropathy
- Drug-induced. This is an uncommon cause, and the molecules most frequently involved are calcium channel blockers and thiazides.
- Institutionalisation (scabies)
- Systemic disease (kidney, liver disease, etc.). These systemic diseases are usually combined. In cases of senile pruritus, we should conduct an interview to investigate any history of general, mental or neurological disease. We should identify any consumption of drugs and alcohol, determine whether there is a risk of STIs, and find out if they are exposed to certain substances as part of their activities.
The clinical examination can detect:
- Pruritus with lesions.
It is easier to manage. The causes range from infectious diseases (scabies, mycosis) to inflammatory diseases (eczema, psoriasis, Grover’s disease), by way of cutaneous lymphoma (be wary of eczema- like lesions on the sides of the body), drug-induced rashes and bullous diseases (BP).
- Pruritus sine materia.
We should consider:
- xerosis, the most frequent cause
- notalgia paraesthetica if the pruritus is localised
- dermatographism
- pre-bullous pemphigoid
- internal diseases (kidneys, liver, cancer). The incidence of cancer is low and the most common cancers are blood cancer and bile duct cancer.
- medications (statins)
- the idiopathic cause.
The assessment proposed by Dr Endo is as follows:
- Examination to look for mites
- CBC, platelets, electrolytes, liver-kidney function tests, thyroid function test, SPEP
- HIV blood test if at-risk individual
- IDIF and DIF
- BP 180/230 ELISA.
In terms of therapy, he recommends:
- Optimising the skin’s barrier function with moisturisers
- Treating the cause if there is one
- If pruritus sine materia is localised: topical agents containing pramoxine, menthol or lidocaine. If this is insufficient, preparations containing ketamine 0.5% / amitriptyline 2.5% (CI for the genital mucosa).
- For generalised pruritus sine materia
UVB phototherapy ++++ (if no risk of falling and no photosensitising medications)
Non-sedative antihistamine only in cases of dermatographism
Gabapentin (100 mg/day, to be used with caution)
- Low-dose naltrexone (1 mg to 4.5 mg/day)
Low-dose antidepressants (mirtazapine 7.5 mg/day, selective serotonin reuptake inhibitor, tricyclic antidepressants)
He never uses the following because they are too expensive or cause a lot of side effects:
- First-generation antihistamines
- Capsaicin
- Medical cannabis
- Thalidomide
- Aprepitant
Some molecules seem promising, such as dupilumab, JAK inhibitors and nemolizumab.
Speaker: Dr. Maria Luisa Perez Cotapos
Report written by Dr. Josefina Marco Bonnet
This was a wonderful photographic presentation of various forms of body art, which has been trendy for several years and is becoming increasingly impressive. We need to be familiar with these trends, which go hand in hand with certain complications.
The following drew my attention:
- The possibility of developing bacterial endocarditis with navel and nipple piercings.
- The increase in conjunctival tattooing. It is not accessible to professional tattoo artists. It is sometimes used by ophthalmologists for aesthetic purposes for patients with corneal opacity or traumatic iridodialysis. The risks are high because in non-ophthalmology settings, it is performed without an ophthalmic microscope and without any strict asepsis technique. The following have been described: pain, blurred vision, photophobia, ink dissemination, granulomas, eyeball penetration, cataracts, retinal detachment, endophthalmitis and blindness.
- The association between tattoos and melanoma. Some authors wonder whether pigment metabolites associated with UV rays may cause the development of melanoma.
- Red pigments are associated with the greatest risk of allergy and complications during tattoo removal.
- Scarification, hot-iron burns, wounds with hot metals, and chemical agents associated with the application of lemon, toothpaste or any other product preventing scarring are new forms of body art. The aim is to obtain a scar.
- Body art is becoming more and more extreme, with lip and tongue tattooing, tongue forking, conjunctival jewellery, navel removal, subcutaneous implants, tooth filing to have pointed teeth, magnetic implants, etc.
As body art is becoming more and more frequent, so are the related complications. We therefore need to be aware of these new trends. We need to educate our patients concerning the risks associated with these new methods. We need to advocate to ensure that these methods are performed by trained professionals, with controlled products and in an aseptic manner.