Acne: Clinic, diagnosis and treatment
Medical editor: Dr. Marina Alexandre, Dermatologist, Avicenne Hospital, France.
Related topics
- Acne / Oily
Key messages:
- Is a chronic inflammatory dermatosis of the pilosebaceous unit.
- Often affects adolescents and young adults.
- It can cause scars but also psychological consequences.
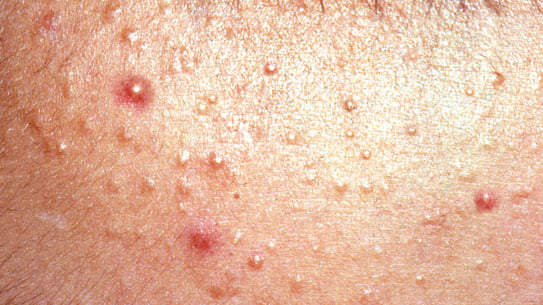
- The diagnosis is clinical: there are two main types of lesions: retentional (microcysts and blackheads) and inflammatory (papules, pustules, and nodules).
- Therapeutic strategy is different according to the type of lesion and its severity.
- The efficacy of the treatments is not immediate, one must be patient.
- Acne is a chronic dermatosis that develops during hormonal changes, particularly during adolescence. It is found in 90% of teenagers and over 40% of adults.
- It affects the sebaceous glands, located at the base of the hair in the hair follicles.
- A dysfunction of these follicles leads to an increased secretion of sebum which leads to a dysfunction of the synthesis of keratin.
- This phenomenon leads to an obstruction of the skin pores and the appearance of acne specific lesions:
- Blackheads, also known as open comedones, or whiteheads, known as closed comedones or "microcysts".
- When bacterial proliferation occurs within closed comedones, they can become inflamed and generate non-purulent erythematous lesions (papules), purulent lesions (pustules) or larger, deeper lesions in the skin (nodules).
Good to know:
- There is a potentially permanent risk of scarring.
- Acne can have psychological consequences, such as mood disorders, depression, lowered self-esteem and relationship difficulties1.
There are several determining factors in the development of acne:
- Hyperseborrhea (increased sebum production by the sebaceous gland): a disturbance of the hormones responsible for the production of sebum (dihydrotestosterone and androgens) or an increased sensitivity of the receptors can be at the origin of the phenomenon of hyperseborrhea2.
- Hyperkeratinization of the follicular Infundibulum: comedones form as a result of an increase in the proliferation of keratinocytes in the pilosebaceous follicle coupled with abnormalities in their differentiation, which leads to an obstruction of the hair follicle canal2.
- Microbial flora and inflammation factors: in acne-prone skin, the anaerobic environment of the sebaceous follicles is dominated by Cutibacterium acnes (formerly known as Propionibacterium acnes3), a Gram-positive bacterium that is over-represented in the microbiome of acne-prone skin. This bacterium is responsible for the production of pro-inflammatory factors at the heart of acne physiopathogenesis2.
- Genetic factors: several studies suggest that there is a genetic background for acne. A history of acne in the first degree increases the risk of developing moderate to severe acne4,5.
The different forms of acne are classified into three categories: common forms, severe forms and specific forms2:
The common forms
Juvenile Mixed Acne
- Most common form of acne.
- Appears at the time of puberty and may extend to the trunk.
- Variable severity:
- Mild or moderate: superficial inflammatory and retentional lesions in varying numbers.
- If nodules are present: severe acne1.
Retentional acne
- Most common form of early acne.
- Manifested mainly by microcysts and open comedones on the face.
The severe forms
Nodular acne or acne conglobate
- Inflammatory nodules that may evolve into abscesses or fistulize deeply (sinuses).
- Frequent extension to the trunk, especially in boys.
- Chronic evolution with often significant scarring.
Acne fulminans (acute, febrile, ulcerative nodular acne)
- Rare.
- Sudden onset.
- Develops more often in boys.
- Associated with altered general condition with hyperthermia at 39-40°C, arthralgias, hyperleukocytosis and multiple inflammatory nodules that may become complicated with necrotic or hemorrhagic ulcerations.
The specific forms
Neonatal acne
- Appears on the face in the first weeks following the infant's birth.
- Regresses spontaneously within a few weeks.
- Is due to maternal androgens.
Prepubertal acne
- Early onset before puberty.
- Mainly retentional.
Exogenous acne
- Prevalence of retentional lesions (open comedones).
- Related to prolonged contact with comedogenic substances, particularly certain mineral oils (massage oils, cosmetic acne, acne mechanica, milling cutters, garage workers, etc.).
Acne in adult women
- Women over 25 years old.
- Juvenile acne lasting into adulthood.
- Rarely, late-onset acne in adulthood.
- Characterized by the predominance of inflammatory papules or nodules located on the lower part of the face.
Acne excoriata
- Almost exclusively found in women.
- Lesions due to repeated manipulation of the facial skin, which is difficult to suppress, leading to erosions.
- Sometimes an indicator of psychological difficulties.
There are 6 levels of acne severity2,6. They are described according to a global severity assessment tool: Global Acne Evaluation (GEA)6.
The different lesions found in acne have been classified as such2,6:
Hyperseborrhea
- Oily and shiny skin appearance.
- Affects areas rich in sebaceous glands: central part of the face (nose, forehead, chin: T-zone, cheeks) and upper thoracic region (back and front of the chest).
- Almost constant.
Retention lesions corresponding to distended pilosebaceous follicles
Two types: closed comedones and open comedones:
Closed comedones (or microcysts)
- Small papules of 2 -3 mm, normal skin color, sometimes more palpable than visible.
- Linked to the accumulation of sebum and keratin mixed in the follicular canal dilated by the obstruction of its orifice.
- Possible secondary inflammation.
Open comedones (blackheads)
- 1-3 mm lesions following the accumulation of keratinocytes and oxidized sebum within the dilated orifice of the infundibular duct.
- Possible secondary inflammation.
Inflammatory lesions
Superficial inflammatory lesions
- Papules: lesions <10mm; often originating from a retention lesion; red, firm and sometimes painful.
- Pustules: usually arise from papules at the top of which appears a yellow purulent content by accumulation of altered polynuclei.
Deep inflammatory lesions
- Nodules: lesions <10 mm.
- May evolve into abscesses and scars.
- Rupture in the depth of the dermis giving sinuses, very painful elongated nodules.
Scars
- 4 types: atrophic, hypertrophic, erythematous, and pigmented.
- Frequent.
- Mostly secondary to inflammatory lesions.
The French Society of Dermatology has established an algorithm7 for the management of acne according to the patient's symptoms. It is described below:
- Do not squeeze/pierce blackheads.
- Apply the topical treatment in the evening to the entire face, not just to the lesions. In the morning, apply a suitable moisturizer. It will improve the tolerance of topical treatments8.
- "Skin cleansers" can only be a possible complement to treatment. To wash, use a mild, foaming, soap-free cleanser. The use of antiseptics, overly aggressive cleansers and mechanical exfoliation are not only useless but can be harmful9.
- Make-up can be applied using "non-comedogenic" products and by carefully removing make-up and by cleansing the skin in the evening.
- Although the sun temporarily reduces the inflammatory nature of lesions, it promotes comedogenesis by thickening the skin. The improvement often observed in the Summer is usually followed by a flare-up in the Autumn.
- Photoprotection is essential when prescribing photo-sensitizing products, especially in the case of dark skin.
- The role of diet in acne is still controversial; it is advisable to avoid ultra-processed foods, fast sugars and large quantities of dairy products10,11.
- The effects of the treatment are not immediate: it takes 3 to 4 weeks to start obtaining results and 3 to 4 months for them to be optimal. Patience and consistency are required.
What treatment can be offered to a pregnant woman?
- Oral isotretinoin, topical retinoids and cyclins are strictly contraindicated. Topical antibiotic treatment may be used: benzoyl peroxide or azelaic acid. Oral zinc can be used from the second trimester onwards1,12.
What to advise to the mother for the acne of the infant?
- Reassure about the always temporary and spontaneously regressive nature of the flare-ups. Advise usual non-irritating hygiene care, no topical antiseptics. Possibly an erythromycin cream in 4% preparation in case of request for treatment.
What contraceptive methods are suitable for this condition?
- As a first-line treatment, either a copper IUD or a second-generation estrogen-progestin is recommended. As a second-line treatment, norgestimate is recommended. If the acne persists after 3 months, consult a gynecologist.
What specific phenomenon explains infant acne?
- Infant acne is due to persistent exposure to maternal hormones.
It seems to me that the copper IUD does not worsen acne and that estrogen-progestins improve it, is this true?
- The copper IUD has no influence on acne, while estrogen-progestogens have a positive or negative influence, depending on whether they are anti or pro-androgenic.
How does the hormonal IUD affect acne?
- In 10 to 15% of cases, it can cause or worsen acne13,14.
What is the difference between papules, pustules, comedones and microcysts?
- A papule is an erythematous lesion that is slightly infiltrated. A pustule has a white tip (cellular debris or pus). A comedo is an open cyst, whereas a microcyst has no opening to the skin.
What is Propionibacterium?
- Propionibacterium acnes is the former name of Cutibacterium acnes. It is a bacterium that contributes to the pathophysiology of acne.
- Acné : quand et comment la traiter ? [Internet]. Haute Autorité de Santé. [website consulted on 08/02/2023].https://www.has-sante.fr/jcms/c_2574402/fr/acne-quand-et-comment-la-traiter
- CEDEF Collège des Enseignants en Dermatologie de France. Dermatologie. 8ème édition. Elsevier Masson; 2022. 471 p. (Les référentiels des Collèges).
- Dictionnaire médical de l’Académie de Médecine [Internet]. [website consulted on 09/02/2023]. https://www.academie-medecine.fr/le-dictionnaire/index.php?q=%3Cem%3ECutibacterium+acnes%3C%2Fem%3E
- Ballanger F, Baudry P, N’Guyen JM, Khammari A, Dréno B. Heredity: a prognostic factor for acne. Dermatol Basel Switz. 2006;212(2):1459.
- Société française de dermatologie. Recommandations de bonne pratique : Traitement de l’acné par voie locale et générale. 10 juin 2015;113.
- Dermatologie SF de. Évaluation de l’acné [Internet]. 2020 [website consulted on 07/02/2023]. https://reco.sfdermato.org/fr/recommandations-acn%C3%A9/%C3%A9valuation
- Société française de dermatologie. algorithme-acné.pdf [Internet]. [website consulted on 07/02/2023]. https://document.sfdermato.org/groupe/centre-de-preuves/algorithme-acn%C3%A9.pdf?ss360SearchTerm=acn%C3%A9
- Levin J. The Relationship of Proper Skin Cleansing to Pathophysiology, Clinical Benefits, and the Concomitant Use of Prescription Topical Therapies in Patients with Acne Vulgaris. Dermatol Clin. avr 2016;34(2):13345.
- National Guideline Alliance (UK). Skin care advice for people with acne vulgaris: Acne vulgaris: management: Evidence review B [Internet]. London: National Institute for Health and Care Excellence (NICE); 2021 [website consulted on 10/02/2023]. http://www.ncbi.nlm.nih.gov/books/NBK573057/
- Penso L, Touvier M, Deschasaux M, Szabo de edelenyi F, Hercberg S, Ezzedine K, et al. Association Between Adult Acne and Dietary Behaviors. JAMA Dermatol. août 2020;156(8):19.
- doi:10.12788/cutis.0565 C 2022 J 16 |. What’s Diet Got to Do With It? Basic and Clinical Science Behind Diet and Acne [Internet]. [website consulted on 10/02/2023]. https://www.mdedge.com/dermatology/article/256058/acne/whats-diet-got-do-it-basic-and-clinical-science-behind-diet-and-acne/page/0/1
- CRAT - Centre de référence sur les agents tératogènes chez la femme enceinte [Internet]. [website consulted on 08/02/2023]. https://www.lecrat.fr/
- Notice patient - MIRENA 52 mg (20 microgrammes/24 heures), dispositif intra-utérin - Base de données publique des médicaments [Internet]. [website consulted on 09/02/2023]. https://base-donnees-publique.medicaments.gouv.fr/affichageDoc.php?specid=66349230&typedoc=N
- HAS, Haute Autorité de Santé. CT-18944_DONASERT_PIS_INS_AvisDef_CT18944.pdf [Internet]. [website consulted on 09/02/2023]. https://www.has-sante.fr/upload/docs/evamed/CT-18944_DONASERT_PIS_INS_AvisDef_CT18944.pdf
Create easily your professional account
I create my account-
Access exclusive business services unlimited
-
Access valuable features : audio listening & tools sharing with your patients
-
Access more than 150 product sheets, dedicated to professionals