Atopic dermatitis: Clinic, diagnosis and treatment
Medical editor: Dr. Marina Alexandre, Dermatologist, Avicenne Hospital, France.
Related topics
- Dryness / Atopy / Eczema
Key messages:
- Chronic and inflammatory skin condition characterized by dry, itchy and eczematous skin lesions.
- Most often occurs in the context of personal or family atopy (asthma, hay fever, allergic conjunctivitis).
- Hygienic and dietary rules compliance, as well as the management of xerosis, are essential in the long term to limit outbreaks.
- Topical corticosteroids are the treatment of choice for flare-ups and should not be dismissed due to excessive corticophobia.
- Topical calcineurin inhibitors may also be prescribed for specific areas.
- In moderate to severe AD, or in case of failure of the dermocorticoids, systemic immunomodulatory treatments or biotherapies can be used, including in very young children, often with great effectiveness.
- One should not hesitate to refer the patient to a dermatologist so that s/he can benefit from these treatments.
- It is important to educate patients and caregivers on how to properly manage and treat AD: proper skin care, identification and avoidance of triggers, as well as adherence to treatment are key. Psychological support and therapeutic education may be helpful.
- Eczema or atopic dermatitis (AD) is a chronic pruritic inflammatory dermatosis that occurs predominantly in infants and children but can persist (or even appear in some rare instances) in teenagers and adults. In France, it affects up to 10 to 20% of infants and young children and about 3.5 to 5% of adults.
- AD is characterized by dry skin (xerosis) associated with skin lesions that progress in flares1.
- Atopy is a group of pathologies related to immune dysregulation of the TH2 pathway including: asthma, allergic rhinitis and allergic conjunctivitis. Approximately 1 out of 2 patients with AD have atopic comorbidities.
- The progression of atopy over the course of the patient's life and the appearance of its successive manifestations is referred to as the atopic march, with AD often being the first manifestation of atopy.
- Atopic dermatitis can significantly affect the quality of life of sufferers due to the severely debilitating itching and the strong psychological repercussions caused by the visible lesions. More than half of all patients are affected by major sleep disorders. The impact on social life is present in almost half of the patients and 43% of patients suffer from anxiety and/or depression1.
- Epidemiological data on AD reveal2:
- A higher prevalence of AD in industrialized countries compared with predominantly rural countries3.
- An increase in the prevalence of AD of approximately 1.8% every 7 years3. In France, the prevalence has more than doubled in 30 years.
- The causes of atopic dermatitis are complex and multifactorial.
- They involve a strong genetic component (with an estimated 75% hereditary transmission4) associated with immune and environmental factors5.
- This heterogeneous disease can be classified according to many criteria depending on morphology, topography, severity, age of onset or course of the disease6.
Genetic factors responsible for the alteration of the skin barrier and immune hypersensitivity
- Mutations in the filaggrin gene (FLG), a major structural protein of the stratum corneum of the epidermis, lead to a functional anomaly of the skin barrier. The skin no longer fulfills its barrier function and becomes permeable to water (xerosis is linked to the inability of the skin to retain water) and to allergens, thus favouring their penetration and interactions with immune cells.
- The FLG mutation is found in nearly 50% of cases of moderate to severe AD in children7 and is associated with an increased risk of developing early AD: x 7.8 risk of developing AD before the age of 5 and x 8.9 risk of developing AD before the age of 20, compared with AD patients without the FLG mutation8.
- Associated with this loss of function of filaggrin, mutations in genes involved in innate and adaptive immunity9 are the main genetic abnormalities observed in atopic dermatitis.
Atopic dermatitis related mutations:
- A 2015 meta-analysis of more than 15 million genetic variants in the journal Nature Genetics identified 10 new markers of risk loci, bringing the known atopic dermatitis risk loci to 31 (24 in European populations).
- The 10 newly identified risk loci are all involved in (auto)immune regulation, in particular innate immune response and T-cell activation and specification10.
Immune system hypersensitivity
- The immune response plays a key role in the physiopathology of atopic dermatitis.
- The penetration of allergens through the altered skin wall leads to an allergic-like TH2 response with the release of numerous pro-inflammatory cytokines, notably IL4 and IL13, and isotypic substitution of B lymphocytes to IgE (immunoglobulin E) antibody-secreting plasma cells.
- Thus, individuals with AD have elevated levels of IgE, leading to hyper-sensitivity to allergens, as well as increased levels of T-cells and pro-inflammatory cytokines such as IL-4 or IL-13. These cytokines are responsible for a reduction in the expression of certain skin barrier proteins independent of any genetic mutation (filaggrin, loricrin and involucrin)11.
- However, it is not required to measure IgE levels to make a diagnosis of AD, which can be entirely based on clinical assessment12.
Good to know:
- Although the primary skin inflammation of AD is not induced by IgE, recurrent allergic reactions causing mast cell degranulation with edematous papules (hives) on the skin will exacerbate AD by increasing inflammation and scratching.
- Because of the increased propensity for induction of specific IgE in AD, allergic reactions to foods are identified in approximately 30% of children with moderate to severe AD12.
Environmental factors that may trigger flare-ups
- Environmental factors, such as respiratory allergens and pollution, contribute to the development of atopic dermatitis. Damage to the skin barrier increases the skin's sensitivity to environmental irritants (pollens, dust, pets, chemicals and irritants such as soaps and cleaners).
- Dry skin makes people with AD more likely to be affected by other environmental factors such as cold, wind and temperature changes...
Infant
- Infant eczema may begin very early (before 2 months old). It evolves in flare-ups, often disappearing by the age of 2, but it may reappear in infancy or later, in adolescence or even in adulthood (less common).
- It usually begins with acute erythema and bilateral desquamation on the cheeks (with respect to the medio-facial area), which may spread symmetrically to the scalp, forehead, perioral area, neck, trunk (with respect to the area protected by a diaper), and extension surfaces such as elbows and knees.
- Less frequently affected parts of the body are the buttocks, the anogenital area, the center of the face and the intertriginous areas.
- Scratching, rubbing, and superinfection may result in lichenification, crusts, and rarely pustules13.
Fig 1,2: Infant eczema
Child
- In childhood (2 to 12 years old), eczema becomes more localized and chronic than in infancy, with paler erythema, xerosis, and poorly delimited lesions usually affecting flexural surfaces with lichenification of chronically affected areas5,13.
- Lesions are generally symmetrical and commonly affect the face, especially the eyelids and ears, as well as flexural surfaces, notably including the elbow and knee creases, the back of the neck, the wrists and ankles13.
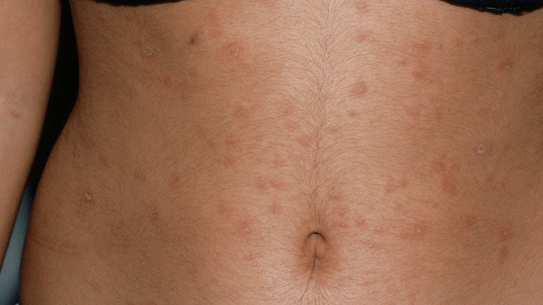
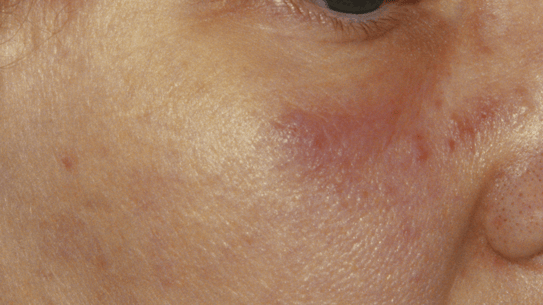
Teenager and adult
- 11 years old marks the start of the teenage or adult stage of AD. Although adolescents and adults usually present with widespread eczema, they may also present with subacute and chronic localized lesions5.
- Commonly affected areas in teenagers are the folds and face, especially the periorbital areas13.
- Adults are usually at risk for erythematous, scaly, sometimes exudative, lichenified or excoriated patches13.
- The distribution of lesions in adults is often localized, usually on the hands (sometimes aggravated by occupational activity), wrist, nipple, bilateral upper eyelids, or lips. However, it may become generalized with increased flexion13.
- On darker skin, the lesions may be hyperpigmented13.
Fig 1,2: Atopic Dermatitis
The diagnosis of AD is clinical and anamnestic. A family history is found in 70% of cases of AD.
The diagnostic criteria defined by the United-Kingdom working party14 can be adopted:
Necessary criteria
Puriginous dermatosis or parents reporting that the child is scratching or rubbing.
Associated with at least 3 of the following criteria
- Personal history of dermatitis of the flexural folds (antecubital fossae, popliteal fossae, anterior surfaces of ankles, neck and/or cheeks) in children younger than 10 years old.
- Personal history of asthma or allergic rhinitis (or atopic disease in a first degree relative in children under the age of 4).
- History of widespread skin xerosis in the previous year.
- Eczema of the folds reaching the cheeks, forehead or convexity of the limbs in children under 4 years old.
- Onset of cutaneous signs before the age of 2 (criterion that can be used for a child over the age of 4).
The differential diagnosis of AD depends on the patient's age, location, and kind of lesions s/he presents with6:
Differential diagnosis based on age
Reference: Raimondo, A. & Lembo, S. Atopic Dermatitis: Epidemiology and Clinical Phenotypes. Dermatol. Pract. Concept. e2021146 (2021).
Adolescent/adult/elderly:
Fig 1: Cutaneous T-cell lymphoma; Fig 2: Pityriasis rosea
Differential diagnostic based on lesion topography
Reference: Raimondo, A. & Lembo, S. Atopic Dermatitis: Epidemiology and Clinical Phenotypes. Dermatol. Pract. Concept. e2021146 (2021).
On the lips:
Fig: Infectious cheilitis
Differential diagnostic based on lesion morphology
Reference: Raimondo, A. & Lembo, S. Atopic Dermatitis: Epidemiology and Clinical Phenotypes. Dermatol. Pract. Concept. e2021146 (2021).
The prognosis for the course and severity of AD are adapted to the age of the patient. While they vary from person to person, there are some general trends:
- In children: most children with AD show significant improvement in their symptoms during adolescence.
- In adults: AD is often less severe in adults than in children, but it can still cause symptoms such as itching and skin lesions.
AD severity scales
The degree of severity of AD can be measured using one of the following scales. In practice, extensive lesions and a significant impact on the quality of life (especially sleep and pruritus) are sufficient to identify severe AD, requiring a referral to a specialist.
Complications from skin infections
- Bacterial superinfection (impetigo): common, due to abnormal colonization of atopic skin by staphylococcus aureus. It is characterized by pustular lesions and yellowish crusts15.
- Viral superinfection: rare but potentially serious (Kaposi-Juliusberg syndrome). A rapid change in the appearance of the lesions with pain, fever, altered general condition that requires an emergency treatment15. The infection is managed by systemic treatment with aciclovir or valaciclovir. It should be started immediately after clinical diagnosis16.
Other complications
- Psychological repercussions can be severe: irritability, sleep disorders, depressive syndrome in children or their parents, significantly affecting quality of life, but also social isolation and emotional development disorders.
- Growth retardation may be observed in infants in very severe cases of AD17.
The treatment for atopic dermatitis is symptomatic.The management and regular monitoring of patients allows:
- To treat the symptoms during the outbreaks.
- To relieve itching.
- To prevent recurrences with appropriate hygienic and dietary advice15.
Background treatment
- Aimed at reducing xerosis, it allows to reduce the dryness of the skin, limit the appearance of flare-ups and restore the skin's barrier function.
- It is based on the daily application of emollients all over the body.
Likewise, the respect of certain hygienic and dietary rules is an integral part of the basic treatment and will limit flare-ups:
- Use mild, soap-free, fragrance-free cleansers with a low detergent content and a physiological pH.
- Wash with lukewarm water (shower rather than bath, not too hot, 35-36°C max), short duration (5-10 min max).
- Dry gently by dabbing with a soft towel15.
- In the case of atopic infants, it may be advisable to shower the child only every other day, cleaning their bottom as often as necessary.
- The addition of bath oil is often practiced, even though its efficacy has not been formally proven15.
- Opt for cotton rather than synthetic clothing15 and any other material that promotes perspiration (nylon, polyamide, tight clothing). Avoid wool (which worsens pruritus).
- In the house, ventilate as much as possible, do not overheat the room in the winter, humidify the atmosphere properly (with a humidifier or with a wet towel spread out across the bedroom floor).
- It is recommended to try and limit contamination by dust, to humidify and to ventilate the rooms.
Good to know:
It is fundamental to explain to the parents (or to the patient) the importance of the daily application of emollients on the whole body by explaining to them that atopic dermatitis is a disease evolving by flare-ups, favoured by the alteration of the cutaneous barrier. It is therefore necessary to preserve and restore it in the long run.
Treatment for flare-ups
Localized treatments
- The treatment of flare-ups is based on the application of dermocorticoids (creams or ointments), once a day on the lesions until they disappear completely15.
- Dermocorticoids make it possible to treat the lesions as and when they appear. It is recommended for them to be used intermittently, as their prolonged use is likely to weaken the skin15.
- The choice of dermocorticoids should be based on the severity of the eczema, its location and the age of the patient:
- Low potency dermocorticoids: are not effective in atopic dermatitis.
- Moderate potency dermocorticoids: can be used on the face and eyelids, folds and seat, including in children and infants.
- Strong potency dermocorticoids: treatment of choice for lesions on the body.
- Very potent dermocorticoids (class I) should not be used to treat children18.
- Areas resistant to dermocorticoids or where there is concern about overly chronic applications, such as the face, can be treated with topical calcineurin inhibitor (tacrolimus).
Systemic treatments
- Very effective, prescribed for moderate to severe AD if topical treatments have failed despite good compliance.
- Ciclosporin, a non-biological systemic immunosuppressant, reserved for severe AD and prescribed by a hospital specialist.
- Monoclonal antibodies targeting cytokines: dupilumab and tralokinumab should be prescribed by a hospital dermatologist, an intern, or an allergologist as a backup treatment when ciclosporin is contraindicated due to failure or intolerance.
- Janus kinase inhibitors: abrocitinib, baracitinib, upadacitinb as a backup treatment in case of failure, or an intolerance or contraindication to cyclosporine.
Other therapeutic approaches
- Phototherapy UVB TL01 with narrow spectrum.
- Phototherapy of PUVA type.
- Patient Therapeutic Education (PTE) sessions.
How to relieve itching?
- Adopt strategies to avoid scratching: use of substitute objects for scratching (fan, thermal water misting, soothing spray, back of a spoon and other rounded objects to rub on the skin...).
- Regular application of emollients and compliance with hygienic and dietary rules should also help relieve itching.
- It may also be recommended to develop stress coping mechanisms to avoid flare-ups.
- Even when pruritus is severe, it is not untreatable. There are now effective treatments for AD (including innovative treatments that can be used in children), so do not hesitate to refer patients to a dermatologist.
Should a specific milk be prescribed for an infant with AD?
- No, providing appropriate therapeutic management is the main priority.
Is there a relationship between iron deficiency in infants and atopic dermatitis? How relevant is iron supplementation to atopic dermatitis?
- There is no link between iron deficiency and atopic dermatitis. An iron deficiency can cause pruritus and xerosis which are not related to atopic dermatitis. Therefore, there is no need to prescribe iron supplements, except in cases of proven deficiency.
Are there barrier creams to allow children to swim in sea water in case of a flare-up?
- There are creams that limit the irritating action of sea water on the skin, but bathing in sea water in a crisis situation is not recommended.
Can we have animals in the house if a member of the household has AD?
- If there is a family history of atopic dermatitis, it is often advisable to avoid introducing a cat into the home when a child is born, but do not deprive yourself of your pet unless you have a proven allergy.
- Simpson EL, et al. "Patient burden of moderate to severe atopic dermatitis (AD): insights from a phase 2b clinical trial of dupilumab in adults." Journal of the American Academy of Dermatology 74.3 (2016): 491-498.
- Suaini NHA, Tan CPT, Loo EXL, Tham EH. Global differences in atopic dermatitis. Pediatr Allergy Immunol. 2021 Jan;32(1):23-33. doi: 10.1111/pai.13335. Epub 2020 Sep 21. PMID: 32841425.
- Odhiambo JA, Williams HC, Clayton TO, Robertson CF, Asher MI. Global variations in prevalence of eczema symptoms in children from ISAAC Phase Three. Journal of Allergy and Clinical Immunology. 2009;124(6):1251-1258.e1223.
- Elmose, C. & Tomsen, S. F. Twin Studies of Atopic Dermatitis: Interpretations and Applications in the Filaggrin Era. J. Allergy 2015, 902359 (2015).
- Langan, S. M., Irvine, A. D. & Weidinger, S. Atopic dermatitis. The Lancet 396, 345–360 (2020).
- Raimondo, A. & Lembo, S. Atopic Dermatitis: Epidemiology and Clinical Phenotypes. Dermatol. Pract. Concept. e2021146 (2021) doi:10.5826/dpc.1104a146.
- Chong AC, Visitsunthorn K, Ong PY. Genetic/Environmental Contributions and Immune Dysregulation in Children with Atopic Dermatitis. J Asthma Allergy. 2022 Nov 23;15:1681-1700.
- Smieszek SP, Welsh S, Xiao C, et al. Correlation of age-of-onset of Atopic Dermatitis with Filaggrin loss-of-function variant status. Sci Rep. 2020;10(1):2721.
- Barbarot, S. & Aubert, H. Physiopathologie de la dermatite atopique. Ann. Dermatol. Vénéréologie 144, S14–S20 (2017).
- The EArly Genetics and Lifecourse Epidemiology (EAGLE) Eczema Consortium. Multi-ancestry genome-wide association study of 21,000 cases and 95,000 controls identifies new risk loci for atopic dermatitis. Nat Genet 47, 1449–1456 (2015). https://doi.org/10.1038/ng.3424.
- Furue M. Regulation of Filaggrin, Loricrin, and Involucrin by IL-4, IL-13, IL-17A, IL-22, AHR, and NRF2: Pathogenic Implications in Atopic Dermatitis. Int J Mol Sci. 2020 Jul 29;21(15):5382.
- Plant A. & Ardern-Jones M.R. Advances in atopic dermatitis. Clinical Medicine. 21(3), 177-181 (2021).
- Chan, C. X. & Zug, K. A. Diagnosis and Management of Dermatitis, Including Atopic, Contact, and Hand Eczemas. Med. Clin. North Am. 105, 611–626 (2021).
- Williams HC, Burney PGJ, Hay RJ, et al. The UK working party’s diagnostic criteria for atopic dermatitis. I. Derivation of a minimum set of discriminators for atopic dermatitis. Br J Dermatol 1994;131:383-96
- Prof. Delphine STAUMONT. La dermatite atopique. dermato info.
- European guideline (EuroGuiDerm) on atopic eczema – part II: non-systemic treatments and treatment recommendations for special AE patient populations.
- Jo, S. Y. et al. (2018) “Common features of atopic dermatitis with hypoproteinemia,” Korean Journal of Pediatrics. Korean Pediatric Society.
- Dermatite atopique de l'enfant - Prise en charge | Recommandations | VIDAL Campus.
Create easily your professional account
I create my account-
Access exclusive business services unlimited
-
Access valuable features : audio listening & tools sharing with your patients
-
Access more than 150 product sheets, dedicated to professionals