Toxidermia: Clinic, diagnosis and treatment
Medical review by Dr. Pierre Schneider, Dermatologist, Saint-Louis Hospital, France
Related topics
- Other
Key messages:
- Toxidermia is defined as a cutaneous adverse drug reaction (CADR).
- Its diagnosis is presumptive. It must be based on clinical and anamnestic arguments.
- It is important to always look for symptoms of severe toxidermia that would require hospitalization.
- Any suspected drug treatment must be stopped immediately and no reintroduction, even for diagnosis purposes, is justified.
- If toxidermia is confirmed, the responsible drug must be communicated to the patient and their physicians pending an allergy evaluation.
- Pharmacovigilance authorities must be notified of any particularly serious or unexpected reactions.
- HIV infection and immunosuppression are very important risk factors for toxidermia.
- Toxidermias are the most common iatrogenic drug reaction.
- Some molecules are more likely to cause toxidermia, but all drugs can be responsible.
- It is therefore necessary to consider all drugs and not only the most common ones.
- Toxidermias can be the consequence of several mechanisms: immunological or not.
- If the cause is not immunological, then it is often possible to predict them based on the different properties of the drug.
- Pharmacodynamic properties may be particularly involved. They can cause xerosis and subretinal cheilitis.
- Nevertheless, non-immunological toxidermia can also be the result of an effect other than the main pharmacological effect sought. Toxidermia can thus be classified into two main categories1 :
1. Non-Immunological Toxidermia
- Dependent on a pharmacodynamic effect of the drug.
- High frequency.
- Dose-dependent.
- Low mortality risk.
- Predictable.
- Detected in controlled trials and post-authorization studies.
- Rarely lead to a market withdrawal but to a modification of the SPCs instead.
2. Immunological Toxidermia
- Dependent on an immunoallergic reaction.
- Rare.
- Not dose-dependent.
- Variable associated rate of mortality.
- Usually occurs within a few days to several weeks after taking the medication.
- Is not predictable.
- Is detected during post-authorization safety studies (PASS).
- May lead to market withdrawal if toxidermia is severe. In all cases, modification of SPCs is required.
Good to know:
Immunological toxidermia can be mediated by two different mechanisms1 :
- Lymphocyte-mediated: These are delayed hypersensitivity reactions (more common) and appear a few days to several weeks after taking the drug. Clinical signs vary in severity, from a simple maculopapular exanthema to toxic epidermal necrolysis (Stevens-Johnson syndrome or Lyell syndrome).
- Mediated by IgE: These are immediate hypersensitivity reactions (rapid onset after taking the drug). They manifest as urticaria, angioedema or anaphylactic shock.
The most frequent forms1,2:
- 40 - 60% of toxidermia present as a maculopapular exanthema.
- 20 - 30% present as urticaria.
Delayed Immunoallergic Toxidermia
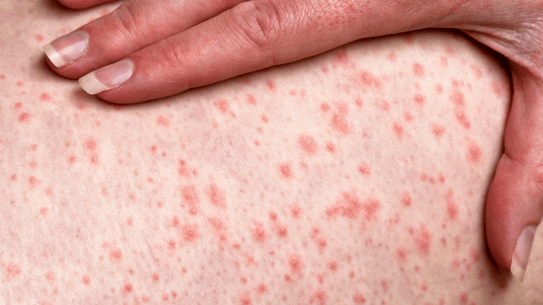
Maculopapular Exanthema - Not severe
- Starts 4 to 14 days after starting medication.
- Initially occurs in the torso or the limb-roots and may progress for a few days.
- Its examination is clinical. Additional examinations may be necessary in case of atypical presentation (possible eosinophilia, renal or hepatic implication).
- It is often manifested by a moderate or absent fever, frequent pruritus of variable intensity and a polymorphism of lesions that may associate:
- Isolated macules, with intervals of healthy skin (morbilliform drug eruption rash).
- Lesions in confluent layers (scarlatiniform eruption).
- Edematous papules or plaques, sometimes with an arciform disposition.
- Petechiae purpura, mostly on the legs and more often in case of intense erythema.
- Usually no enanthema (mucosal involvement).
- It generally evolves favorably in 1 week to 10 days after stopping treatment.
Fixed Erythema Pigmentosum - Not severe
- Pathognomonic of toxidermia: It is the only dermatosis of almost exclusively drug origin.
- Starts within 48 hours of taking the medication (often NSAIDs or paracetamol).
- Manifested by 1 to 10 rounded erythematous macules, a few centimeters in diameter, located preferentially but not exclusively on the genitals and lips. These macules are often painful and infiltrated and may develop into plaques.
- Possibility of bullous and generalized evolution.
- Inflammatory lesions usually resolve within a few days but may leave pigmented spots.
- If the responsible drug is reintroduced: rapid recurrence in the same locations.
Fig: Fixed erythema pigmentosum
Acute Generalized Exanthematus Pustulosis (AGEP) - Severe
- Manifested by a severe and very febrile rash, can be mistaken for an infection.
- Usually begins 1 to 11 days after taking medication (often antibiotics) with fever, a scarlatiniform, sheet-like erythema, predominantly in the large folds.
- In only a few hours, appearance of small amicrobial pustules with lactescent content on the whole erythema.
- Although this reaction can occur in all individuals, it is less common in children and thus may manifest itself atypically3.
- Symptoms regress rapidly when the medication is stopped (about 2 weeks3).
- The pustules disappear within a few days with a diffuse desquamation.
Drug Hypersensitivity Syndrome or DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms) - Severe
Rare. Recognized by several criteria:
- Severity and extent of the rash (often more than 50% of the body surface), sometimes erythrodermic (more than 90% of the surface).
- Infiltrated rash: oedema of the face and of the extremities is an important and characteristic clinical sign.
- Severe pruritus.
- High fever.
- Diffuse adenopathies.
- If visceral damage, possible life-threatening complications.
Fig 1,2,3: DRESS Syndrome
Among the drugs implicated in DRESS, the most frequently suspected are:
- Anti-epileptic medication (phenobarbital, carbamazepine, phenytoin, lamotrigine).
- Minocycline, allopurinol, dapsone.
- Some antiretroviral drugs such as nevirapine and abacavir.
- Sulfonamides such as sulfasalazine, sulfadiazine and sulfamethoxazole.
- Gold salts and proton pump inhibitors2,4.
Good to know:
- It usually takes 2 to 6 weeks from the start of treatment to the onset of symptoms.
- The delay is sometimes shortened for certain antibiotics or iodinated contrast products.
- The rash may persist for several weeks, with a slow regression.
- Cutaneous and/or visceral outbreaks may occur repeatedly in the weeks and months following the onset, often associated with viral reactivations.
Stevens-Johnson Syndrome (SJS), Lyell Syndrome (Toxic Epidermal Necrolysis or TEN) - Severe
- The most severe forms of toxidermia are those that present a continuum between Stevens-Johnson syndrome and Lyell-TEN syndrome, distinguished primarily by the surface area of affected epidermis.
- These forms are considered medical emergencies.
- The same drugs can cause different levels of severity, and in many patients, the rash can spread rapidly from Stevens-Johnson syndrome to LYELL syndrome in just a few days.
- Genetic background is a risk factor for these diseases5.
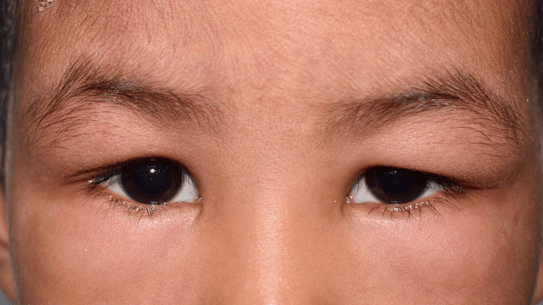
- The first signs usually appear between 4 and 28 days after the introduction of the inducer, with mucocutaneous symptoms such as fever, burning eyes, pharyngitis and a painful erythematous rash.
- The prodromal phase develops rapidly over hours to days, with multifocal mucosal erosions and skin bullae, as well as Nikolsky's sign where epidermal flaps detach upon rubbing.
- Stevens-Johnson syndrome is distinguished from Lyell-TEN syndrome by the area of necrotic epidermis (less than 10% for the former and more than 30% for the latter)6.
- Patients have a fever and a severely altered general condition and may suffer from visceral involvement such as necrosis of the bronchial or the intestinal epithelium.
- Complementary biological tests may be performed to confirm the diagnosis: leukopenia, signs of multivisceral failure, hydroelectrolytic disorders.
Fig 1: Stevens-Johson Syndrome; Fig 2: Lyell-TEN Syndrome
The mortality risk for this toxidermia is high: 4.8% for SJS, 19.4% for SJS-TEN overlap and 14.8% for TEN6. Re-epidermalization occurs within 10 to 30 days, with frequent sequelae: pigmentation disorders and mucosal scars, especially in the eyes (synechiae).
For more information:
Epidemiological case-control studies conducted in Europe by EuroSCAR2 have identified the drugs responsible for Stevens-Johnson syndrome and toxic epidermal necrolysis, namely antibacterial sulfonamides, allopurinol, carbamazepine, phenobarbital, phenytoin, non-steroidal anti-inflammatory drugs of the oxicam family and, to a lesser extent, nevirapine, lamotrigine, sertraline, pantoprazole and tramadol6.
Urticaria
- Mobile and fleeting pruritic edematous papules emerging a few minutes to a few hours after the drug is taken.
- If immediate hypersensitivity reaction is IgE-mediated (reflects previous sensitization): does not occur on first contact with the drug.
- This definitely contraindicates further use of the same drug.
- If reactions are related to the properties of the drug: constant in the same person and dose-dependent.
- Less than 10% of acute urticaria have a drug-related origin.
Fig 1,2: Acute urticaria
Angioedema and Anaphylactic Shock
Superficial and/or deep urticaria may, in rare cases, be associated with an episode of anaphylaxis.
- Respiratory signs: dysphonia, dyspnoea, bronchospasm.
- Cardiovascular signs: tachycardia or bradycardia, arterial hypotension.
- Digestive signs: nausea, vomiting, diarrhoea.
- Any anaphylactic reaction requires emergency treatment.
Photosensitivity
Rash occurring within hours of exposure to the sun. Localized on the exposed areas: photodistribution.
It depends on two distinct mechanisms:
1. Photoallergy
- Manifested as eczema lesions in exposed areas but may spread.
- May be caused by minimal sun exposure.
- Occurs between 7 and 21 days after the start of treatment.
- May be secondary to systemic or topical treatment.
2. Phototoxicity
It occurs in the hours following sun exposure.
Diagnoses are most often clinical, but additional biological tests may be performed in some cases.
As toxidermia manifests itself in multiple forms depending on the individual and the drug, each reaction has its own differential diagnosis. The main differential diagnoses referenced concern immunoallergic toxidermia.
Maculopapular Exanthema
These rashes can also have an infectious origin: in children, 70 - 80% of exanthemata have an infectious cause.
Acute Generalized Exanthematus Pustulosis (AGEP)
Generalized pustular psoriasis characterized by a less abrupt onset, more prolonged evolution and the need for a history of psoriasis.
Drug Hypersensitivity Syndrome or DRESS
- Other causes of erythroderma: psoriasis, eczema, epidermotropic T-cell lymphomas (such as mycosis fungoides and Sézary syndrome), but these causes can be ruled out by history, skin histology, and count.
- Primary or secondary hypereosinophilic syndromes usually have a less acute onset.
Stevens-Johnson Syndrome or SJS
- May be confused with erythema multiforme, which is a rare disease characterized by eruptive lesions in the form of a rosette or bullseye, often symmetrical and acral, with frequent mucosal erosive lesions.
- Recurrences are frequent.
- They are often caused by recurrent herpes, especially labial, but can also be caused by other infectious diseases such as Mycoplasma pneumoniae.
Lyell Syndrome (Toxic Epidermal Necrolysis or TEN)
Must be differentiated from other pathologies such as:
- Staphylococcal epidermolysis, which mainly affects infants: without mucosal erosions and with superficial skin detachments often located around orifices and large folds, subcorneal detachments on histology. Staphylococcal epidermolysis has a good prognosis under antibiotic treatment.
- Autoimmune bullous dermatosis: without necrosis of the epidermis, with antibody deposits observed in direct immunofluorescence.
- Burns: do not result in mucosal lesions and have a variable depth of skin necrosis.
Determine the Liability of the Triggering Medication
- List all medication taken in the previous weeks, including those considered negligible by the patient: aspirin and other analgesics, nasal drops, sedatives, laxatives, fortifiers, suppositories, lozenges, etc.
- Establish the precise chronology of these different drug intakes in relation to the onset of the rash.
- Clinical analysis.
These three elements make it possible to determine the therapies involved and to proceed to their immediate interruption. These drugs are contraindicated for use by this patient.
Treatment of toxidermia
Severe forms
Hospitalization in a specialized care center for specific treatment.
Minor forms
Antihistamines, local corticosteroids and sometimes general corticosteroid therapy (erythroderma and DRESS).
More than 90% of toxidermia is benign. Only 1/10,000 to 1,000,000 are life-threatening.
- Consult a dermatologist: they will immediately suspect drug-induced toxidermia, determine its origin and judge its severity and the need for hospitalization. They may report the case to the pharmacovigilance center.
- Reassure the patient: in the most common forms of toxidermia, the regression of the symptomatology is rapid and without sequelae after stopping the responsible drug.
- Explain:
- The treatments put in place are symptomatic. It is the cessation of the medication that is imperative.
- The specific list of medications to be contraindicated in the future for the patient.
- The uselessness and danger of allergy tests or of the reintroduction of the suspected drug.
Can toxidermia affect the pregnancy? Can it have an impact on the delivery or the child?
- It is important to note that, in practical terms, the toxicity would be related to a drug that is contraindicated during pregnancy. Mild toxidermia has no consequences. On the other hand, all severe toxidermia, because of the intensity of the general signs, are of course detrimental.
Should I contact the doctor?
- Yes, as soon as possible to confirm drug discontinuation and obtain alternative therapy.
Does toxidermia occur every time I take medication?
- Once a toxidermia occurs, it will recur with each dose of the drug. However, it does not always occur with the first dose.
Is an appointment with an allergist necessary?
- The ideal scenario is to make an appointment with an allergist to explore the specific allergenic molecule. Tests should usually be scheduled in a hospital setting.
Can a simple toxidermia reveal a higher risk of developing severe toxidermia?
- The severity of toxidermia can vary from one intake to another.
Is toxidermia usually triggered by the first dose or by the 2nd or 3rd?
- Toxidermia rarely occurs upon the first intake; it requires contact with the allergen for the body to synthesize antibodies that cause toxidermia.
- DEF Collège des Enseignants en Dermatologie de France. Dermatologie. 8ème édition. Elsevier Masson, 2022.
- Lebrun-Vignes B, Valeyrie-Allanore L. Toxidermies. Rev Médecine Interne 2015; 36: 256–270.
- Speeckaert MM, Speeckaert R, Lambert J, Brochez L. Acute generalized exanthematous pustulosis: an overview of the clinical, immunological and diagnostic concepts. Eur J Dermatol EJD 2010; 20: 425–433.
- Choudhary S, McLeod M, Torchia D, Romanelli P. Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) Syndrome. J Clin Aesthetic Dermatol 2013; 6: 31–37.
- Noe MH, Micheletti RG. Diagnosis and management of Stevens-Johnson syndrome/toxic epidermal necrolysis. Clin Dermatol 2020; 38: 607–612.
- Oakley AM, Krishnamurthy K. Stevens Johnson Syndrome. StatPearls Publishing, 2022 https://www.ncbi.nlm.nih.gov/books/NBK459323/ [Consulted on 27/02/2023].
Create easily your professional account
I create my account-
Access exclusive business services unlimited
-
Access valuable features : audio listening & tools sharing with your patients
-
Access more than 150 product sheets, dedicated to professionals